Why do cancer patients lose so much weight?
Cancerous tumors have long been known to reprogram metabolic processes within and around themselves in order to obtain a steady supply of essential nutrients. But in recent years, researchers have come to realize that cancer can also alter metabolic processes systemically, throughout the patient’s body. Among the grave consequences of this is ‘wasting syndrome’—rapid weight loss that is unconnected to the patient’s diet and cannot be offset by high caloric intake. This syndrome occurs in cancer patients whose body metabolism is thrown far out of whack.
A new study, led by Prof. Ayelet Erez from the Department of Molecular Cell Biology, has revealed how cancerous tumors trigger wasting syndrome. The scientists propose a method for predicting cancer-caused weight loss and point the way toward developing possible treatments.
They focused on the liver—the body’s metabolic hub—with a focus on the urea cycle. Through the urea cycle, the body rids itself of excess nitrogen by having it transferred to the liver as ammonia, converted into urea, and then excreted from the body in urine. The Erez team had previously discovered that low urea levels in urine could signal the presence of cancer; as the cycle starts malfunctioning, the cancer cells soak up the excess nitrogen for their own growth purposes, leaving less to be excreted in urine.
Now, using mouse models of human breast and pancreatic cancers, the scientists demonstrated that interference with the urea cycle triggered a build-up of amino acids in the blood. The tumors then used these amino acids to assemble their own RNA and DNA. Furthermore, as the urea cycle faltered, excess ammonia also accumulated (a nitrogen-based byproduct), impairing the ability of the body’s immune cells to fight back.
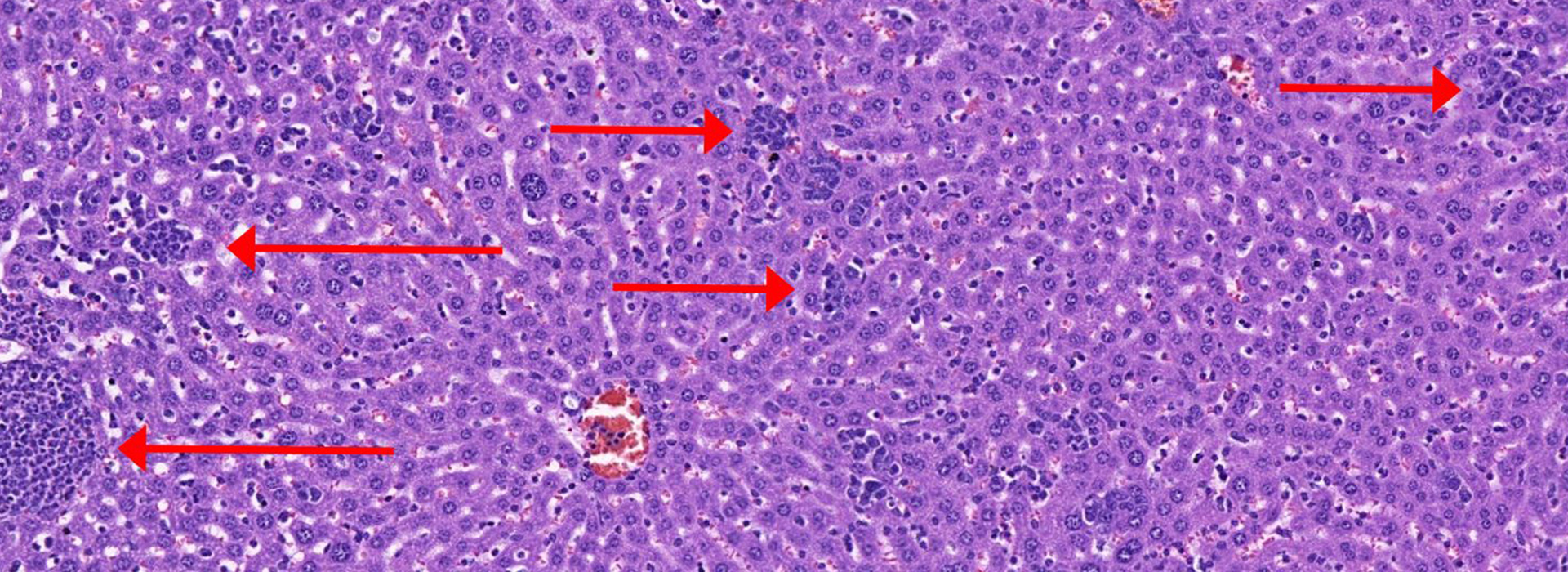
How is cancer able to reprogram metabolic processes in the liver? Prof. Erez and her team discovered that coincidental with metabolic changes in the liver, certain types of immune cells start infiltrating the liver—white blood cells released into the blood stream as part of the inflammatory response intended to fight the cancer. As the cancer progresses, the liver fills up with large numbers of mature, active white blood cells called neutrophils and monocytes.
That might sound like a good thing, but it isn’t. Using RNA sequencing techniques at different stages of disease, the Erez group showed that as the white blood cell count rises, the liver stops producing a key protein known as HNF4α, a master regulator of metabolic processes, and limits its production of the protein albumin, which is critical to preventing swelling and leakage from blood vessels. When levels of HNF4α and albumin dropped, the mice started losing weight.
Using gene therapy to increase the levels of these proteins prevented weight loss, shrank tumors, and increased survival.
These findings provided strong evidence that the wasting syndrome is caused, at least partly, by a decrease in the metabolic master regulator HNF4α, brought on by immune cells infiltrating the liver. The research also raises the hope that in the future, it might become possible to prevent or even treat this syndrome. This study appeared in the July 2023 issue of Cancer Discovery.

Prof. Ayelet Erez is Head of the David and Fela Shapell Family Center for Genetic Disorders Research and the incumbent of the Sir Ernst B. Chain Professorial Chair. Her research is supported by the Koret Foundation, and the Dr. Gilbert S. Omenn and Martha A. Darling Weizmann Institute - Schneider Hospital Fund for Clinical Breakthroughs through Scientific Collaborations. The Blumberg Family Research Fellow Chair in Honor of Talia Lynn Steckman supports a staff scientist in Prof. Erez’s lab.