A potent future for stem cells
From reprogramming to creating new tissues and organs
Features
What exactly are stem cells—and what promise do they hold for human health? Stem cells are early-stage cells that have the potential to develop into any type of cell—which is why they are often referred to as pluripotent and can become muscle cells, blood cells, brain cells, and so on.
The medical implications are far-reaching. Being able to take a group of these cells that contain the building blocks necessary to become any cell in the body creates the real possibility for scientists to fabricate any healthy tissue to replace damaged or diseased organs. With perhaps some of the most visionary and versatile applications in regenerative medicine today, a clear understanding of stem cells is now central in research on heart disease, cancer, bone marrow transplants, and beyond.
At the Weizmann Institute, scientists are opening new avenues in the study of stem cells, finding ways to reverse, suspend, or continually change cell maturation. Here are some of the research avenues.
Back to basics
A key hurdle in stem cell research was precluding the use of embryos, and Prof. Yaqub Hanna in the Department of Molecular Genetics has been at the forefront of the worldwide effort to reprogram human skin cells to a stem-cell-like state.
After conducting his postdoctoral research at MIT, in one of the world’s leading stem cell labs, Prof. Hanna successfully created induced pluripotent stem cells (iPSCs)—reprogrammed mature cells that have the potential to differentiate into any cell type—from skin cells. Until now, the success rate for creating iPSCs has been around 10% and took between two to four weeks. but Prof. Hanna and his team figured out how to revert adult skin cells to iPSCs 100% of the time and in only eight days. This quick and efficient method was his unique breakthrough. This discovery catapults forward the efficiency of cell reprogramming into new, exciting territory and may eventually lead to major advances in tissue engineering and regenerative medicine.
Currently, Prof. Hanna is applying these techniques to bring about personalized stem-cell therapies to men and women facing the challenge of infertility and has already successfully generated human iPSCs that could be nudged genetically to differentiate into progenitors of sperm and egg cells in culture in only six days.
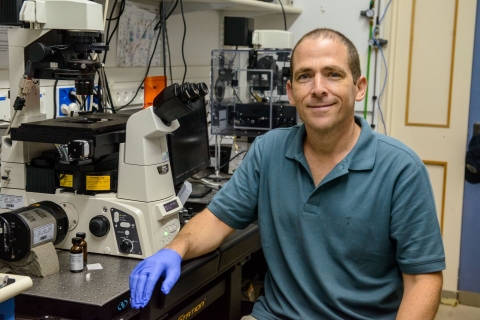
Dr. Yonatan Stelzer, who did his postdoctoral research in the same MIT lab, has been working together with Prof. Hanna to create these efficient induced pluripotent stem cells and explains the process. “Stem cells and development are a one-directional progression, where cells acquire their fate like a rock at the top of a hill that has a lot of action potential,” he says. “Once it starts rolling down, it loses its potential and starts going down these bifurcated routes. The concept of iPSCs shows that we can essentially push this stone back up to the top of the hill so we can reacquire all its decisions again.”
How does a stem cell differentiate?
Cells have the potential to become one of 220 types in the body—but they all begin as stem cells. What determines their fate?
Stem cell differentiation and cell-fate decisions are shaped by complex layers of epigenetic modifications that specify, memorize, and modulate functional embryonic programs. Epigenetics deals with how, and in which cell type, specific genes are expressed—whether they are active or inactive. Using his postdoc research where he created a synthetic sensor that, for the first time, allowed for the visualizing of epigenetic changes as they occur in real time, Dr. Stelzer, a member of the Department of Molecular Cell Biology, is currently focusing on single-cell level phenomenological characterization of embryonic cell-fate decisions to understand how epigenetics play essential and instructive roles during these fundamental processes.
By decoding how cells differentiate on an epigenetic level, he hopes to learn how this key process can go awry, and lead to diseases and cancer. Building on knowledge gained from normal embryonic development, Dr. Stelzer will be able to program stem cells into different cell types, which potentially has monumental implications for regenerative medicine.
In the Department of Biological Regulation, Prof. Atan Gross has been exploring this question from a different direction. Studying MTCH2, a protein he discovered over a decade ago, Prof. Gross and his team found that when stem cells had a copy of the so-called “Mitch” gene, its mitochondria fused together at a high rate, creating larger mitochondrial structures.
The elongated mitochondrial cells proceeded to differentiate. Conversely, in stem cells that they genetically engineered to lack the gene, the mitochondria did not fuse as frequently, and remained in a stem cell state as a result. Being able to control whether or not a stem cell differentiates into a mature cell by modulating its mitochondrial morphology and metabolism presents scientists with new possibilities, offering a major step forward in this field.
Is a stem cell’s fate set in stone?
Until now, scientists have assumed that these differentiated cells acted as any other—once the stem cell has matured, its transformation is over and its makeup set. Prof. Shalev Itzkovitz recently discovered that, in fact, this is not the case: they can keep changing. A member of the Department of Molecular Cell Biology, Prof. Itzkovitz has been studying the hundreds of millions of new cells that are born every day in the small intestine. Traveling up the surface of small stalagmite-like protrusions on the inner intestinal wall called the villi, these cells have a lifespan of four days before reaching the villi tip and being discarded.
Using a sequencing method called “laser capture” to create a detailed map of these cells, Prof. Itzkovitz found that as the cells travel up the villi, they continue to differentiate in order to fulfill different functions based on their location. Continuing to explore this discovery and analyzing the difference between healthy and diseased gene expression with regard to cell location in the villi may shed light on what causes inflammatory bowel diseases.
These findings have an impact on more than just the small intestine. The sequencing methods developed by Prof. Itzkovitz’s research team can be applied to creating detailed atlases of cells in various body tissues, and even in tumors.
A whole new era of medicine is being made possible through stem cell research. By learning how to reprogram human cells, scientists are hoping to create a method where the body cures itself, rather than relying on external and often ineffective medications.
Do stem cells have internal clocks?
Stem cells in the bone marrow replenish the blood daily with billions of short-lived mature blood and immune cells. Research conducted by Prof. Tsvee Lapidot in the Department of Immunology has now demonstrated that stem cells retained in the marrow follow daily cycles of light and darkness. This discovery suggests that adjusting the timing of stem cell harvesting—or the administration of the sleep hormone melatonin—may help increase the success of clinical bone marrow transplantation protocols.
Measuring the levels of blood-forming stem cells in the marrow of mice over a period of 24 hours, Prof. Lapidot’s team found two peaks in stem cell production: one at 11:00 am and the other at 11:00 pm. They found that, during the daylight morning peak, large numbers of stem and progenitor cells were maturing, differentiating into the various types of mature blood and immune cells required for replenishing the blood. During the night peak, on the other hand, the majority of stem cells in the marrow were undifferentiated stem cells—a state maintained in response to melatonin.
Because the night peak was characterized by a greater number of undifferentiated stem cells, bone marrow transplantations with stem cells obtained at night were superior to those with stem cells obtained in the daytime. Moreover, the cells engrafted the bone marrow of recipient mice more than twice as efficiently as stem cells collected during the morning peak. The scientists also found that pretreatment of the stem cell donors with melatonin for a few hours during the day increased the recipients’ stem cell repopulation potential following bone marrow transplantation.
The findings of this study suggest that, in human patients, it might be possible to increase the success of transplantations by pretreating bone marrow donors with melatonin, or with other molecules found to regulate the light and darkness cycles of stem cell production.
The team’s discovery may offer a strategy for increasing the efficacy of transplantation procedures performed on elderly patients, as people over the age of 60 experience a sharp decline in melatonin production.
Prof. Yakub Hanna is supported by the Nella and Leon Benoziyo Center for Neurological Diseases, the David and Fela Shapell Family Center for Genetic Disorders Research, the Kekst Family Institute for Medical Genetics, the Helen and Martin Kimmel Institute for Stem Cell Research, Helen and Martin Kimmel Award for Innovative Investigation, Pascal and Ilana Mantoux, Edmond de Rothschild Foundations, Zantker Charitable Foundation, Rachel Peles, Estate of Zvia Zeroni, and the European Research Council.
Prof. Atan Gross is supported by the Rising Tide Foundation and the Estate of Emile Mimran. He is the incumbent of the Marketa & Frederick Alexander Professorial Chair.
Prof. Shalev Itzkovitz is supported by the Wolfson Family Charitable Trust, the Edmond de Rothschild Foundations, and the European Research Council.
Prof. Tsvee Lapidot is supported by the Helen and Martin Kimmel Institute for Stem Cell Research, the Felix and Silvia Schnur Endowment Fund in Stem Cell Research, the Dr. Beth Rom-Rymer Stem Cell Research Fund, the Henri Gutwirth Fund for Research, the Hadar Impact Fund, and Asher Pertman and Wayne Pertman. He is the incumbent of the Edith Arnoff Stein Professorial Chair in Stem Cell Research.
Dr. Yonatan Stelzer is supported by the Benoziyo Fund for the Advancement of Science, the Helen and Martin Kimmel Institute for Stem Cell Research, and the Jean - Jacques Brunschwig Fund for the Molecular Genetics of Cancer. He is the incumbent of the Louis and Ida Rich Career Development Chair.
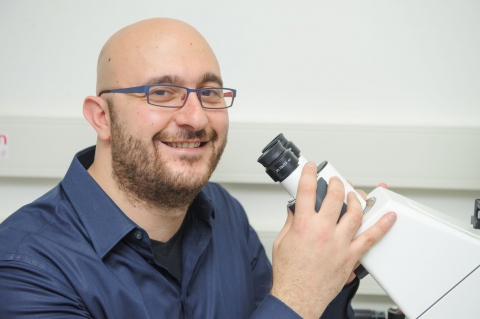
Prof. Yaqub Hanna

Dr. Yonatan Stelzer

Prof. Atan Gross
Prof. Shalev Itzkovitz

Prof. Tsvee Lapidot