The Bench-to- Bedside Project
Big data, the genomics revolution, and a new era in medicine
Features

Two of the most exciting scientific revolutions of our time—genomics and big data science—promise to usher in a new era characterized by rich, sensitive, personalized, and adaptive medicine.
To that end, the Weizmann Institute of Science and Clalit Health Systems—Israel’s largest health maintenance organization (HMO)—are launching a joint research program that will leverage the availability of patient data for the benefit of scientific research and clinical care. The program, which is the central feature of the new Bench-to-Bedside Project, represents a major step in linking a world-leading scientific research institution with a world-leading big data repository providing medical records on more than half of the Israeli population.
The project aims to engage scientists and physicians in shaping new medical research paradigms by harnessing modern mathematical and statistical modeling of millions of patients’ genomic profiling data, leading to improved diagnosis and personalized treatment protocols.
“The Weizmann-Clalit program is a major step in the rapid transformation we see in the way biomedical research is being carried out,” says Weizmann Institute President Prof. Daniel Zajfman. “It will allow scientists to link the work done at the bench more directly with the bedside. The ability to link the knowledge in such a medical database with scientific results in the laboratory has the potential for speeding up scientific discoveries in many fields of the life sciences.”
“This is a highly unique translational research collaboration that is certain to yield major insights in a range of biomedical specialties,” says Prof. Gabi Barbash, MD, MPH, who has joined the Weizmann Institute to direct the Bench-to-Bedside Project (see below).
His first task will be to coordinate four "pioneering projects" utilizing the Clalit database: two on diabetes, one on multiple myeloma, and one on human phenotypes. Each will bring together advanced analysis of anonymized medical records and innovative Weizmann Institute-made genomic analyses of select patients. Prof. Barbash expects that these projects will pave the way to an even broader initiative, leading to the broad sequencing of 100,000 genomes of Israelis, a $100 million initiative called the “IL100K” project, which, he says, “could change the face of patient care in Israel and hopefully serve as a model for other healthcare systems.”
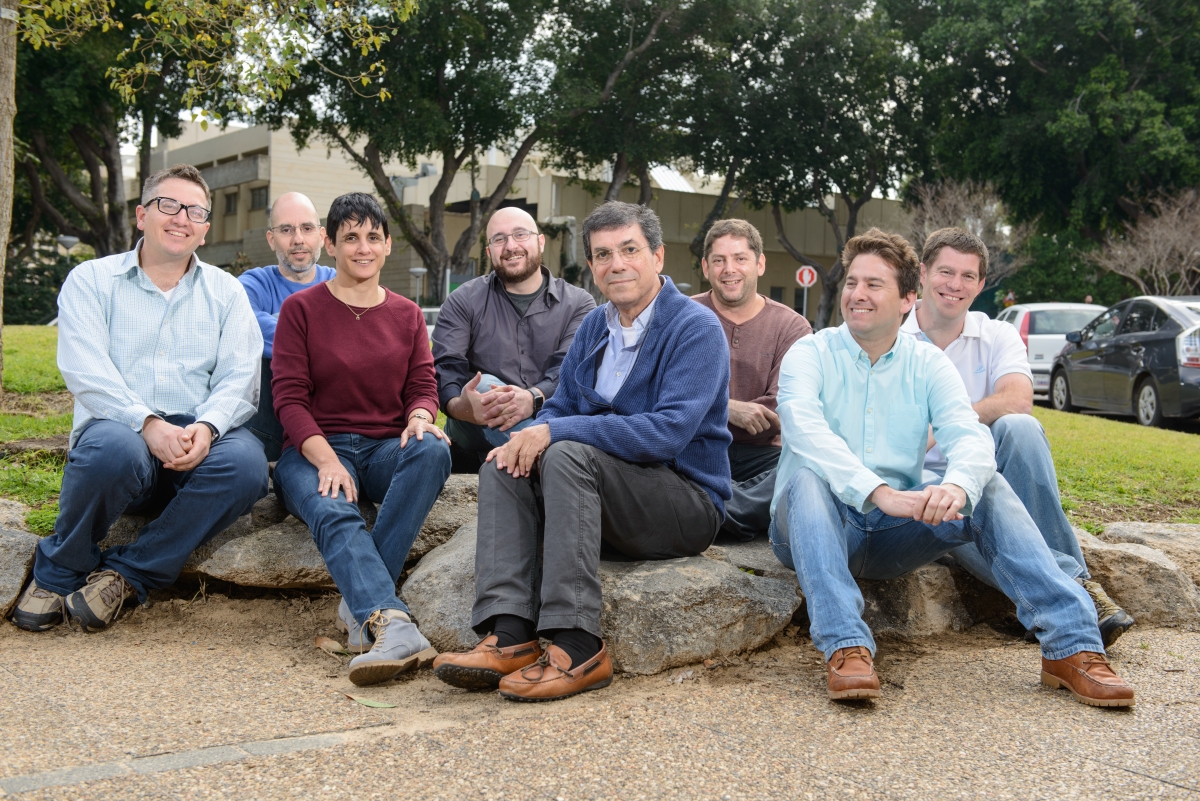
Prof. Amos Tanay, of the Department of Biological Regulation and the Department of Computer Science and Applied Mathematics, is working with Prof. Barbash to establish the project, and is co-leading one of the four pioneering projects (on multiple myeloma).
“Beyond the exciting opportunity in applying our genomics tools to key common disease, we believe that providing the Weizmann Institute research community with access to the Clalit’s data can be truly transformative,” he says. “We cannot predict which insights our scientists will generate from this treasure, but we expect novel and paradigm-changing discoveries in both basic science and practical healthcare applications,” says Prof. Zvi Livneh, Dean of the Faculty of Biochemistry.
Converging basic science and clinical care
Doctors and scientists alike are used to observing disease processes, hypothesizing about origins of diseases and potential cures, testing these ideas in experiments, and making decisions based on additional data. However, unlike today’s decisions, which are typically based on a few dozen tests within a standard blood workout, tomorrow’s medical decisions will likely take into account millions of patient-tailored data points that are derived from modern genomic technologies. Combining all patient data— including clinical records and genetic data—into one coherent and trustworthy medical tool requires an entirely new set of interdisciplinary methods. These should incorporate concepts from mathematics, computer science, and modern biology into clinical knowledge. Synthesis of ideas can happen only if physicians and scientists come together to develop such tools jointly, points out Prof. Barbash.
“We believe immediate action is needed in order to transform the potential of clinical genomics research in Israel into a real engine of research and innovation, for the benefit of medical research, and healthcare innovation,” he says. “The window of opportunity is narrow, since within a few years, several competing initiatives in the world might set standards and establish leadership in this young field.”
Building a framework allowing such exchange is not an easy task, but both the Institute and Clalit are exceptionally positioned. First, the unique structure of the healthcare system in Israel - just a few HMOs in a compact country with a socialized healthcare system - means that much of the data is centralized. Indeed, over the last 20 years, Clalit has processed and stored its medical data for over half of the Israeli population.
Meanwhile, the Weizmann Institute is a world leader in genomics, starting from the earliest days as a key participant in the Human Genome Project in the 1990s. That initiative spawned a wide range of research avenues, and Institute scientists have gone on to explore the molecular and genetic mechanisms that underlie basic biological processes in complex organisms, addressing a wide range of biological questions. In addition, Weizmann Institute scientists have world-renowned expertise in bioinformatics and systems biology. In addition, the Nancy and Stephen Grand Israel National Center for Personalized Medicine has quickly become a nationwide hub for transformational research that integrates genomics, protein profiling, bioinformatics and drug discovery.
In the long term, the infrastructure created by the initiative will be made accessible to the entire spectrum of medical researchers—from data analysts and machine learning experts to medical doctors and scientists throughout Israeli academia, above and beyond the Weizmann-Clalit initiative.
“The Bench-to-Bedside Project will strive to develop a major, nationwide clinical genomics initiative, a domain in which the Israeli system may have an edge over other healthcare systems like in the U.S., the UK, and the EU,” says Prof. Barbash. “Our projects will set new standards in integration of clinical data and genomic analysis, and in the long run, we believe we can transform the potential of clinical genomics research in Israel into a major engine of research and innovation for the benefit of patients and the entire healthcare system.”
“Combining the Weizmann Institute’s state-of-the-art research capabilities with the immense patient base from Clalit represents a strategic opportunity to join forces in incorporating big data approaches into the clinical patient care scheme,” says Dr. Eran Elinav of the Department of Immunology, a medical doctor who is involved in one of the four pioneering projects. “As such, the fruits of this alliance may enable the diagnosis, prevention, and treatment of common disease by integrating human genomic and microbiome features into the personalized medicine field. The growing number of Weizmann scientists holding a medical degree may help to form the bridge making this vision a reality.”
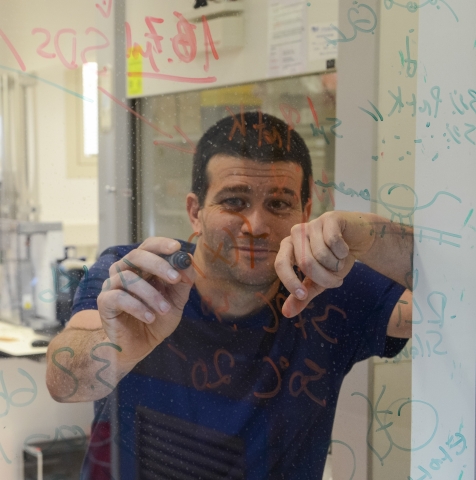
Prof. Gabi Barbash: Director of the new
Bench-to-Bedside Project
In his 18 years as director of Tel Aviv Sourasky Medical Center, one of Israel’s largest hospitals, Prof. Gabi Barbash managed medical crises, oversaw an emergency room that treated victims of terror attacks, supervised a vibrant clinical research program, and grappled with some of the most vexing challenges in healthcare. He accompanied the trauma teams as they tried to save the life of Prime Minister Yitzhak Rabin when he was brought to the ER unit after being shot on the night of Nov. 4, 1995.
Prof. Barbash served in that role until last year. For three of those years (1996-1999) he served as Director General of Israel’s Ministry of Health. I 1997, he launched a nationwide program to control an outbreak of tuberculosis after a dramatic surge of new cases occurred with the arrival of a large number of immigrants from the former Soviet Union and Ethiopia. That required orchestrating all four of Israel’s health maintenance organizations (HMOs) to cooperate in controlling the reemergence of this disease.
When it became evident that Israel has one of the highest rates of breast cancer in the world, he introduced nationwide mammography screening for women over age 50.
As chairman of the Israeli National Transplant Center (1998-2000), he reorganized the system of organ harvesting, doubling the number of organ transplantations in Israel. The transplantation revolution was a particular challenge in Israel, where religious beliefs in addition to other factors inhibit families from donating the organs of their loved ones.“What I discovered when I looked into the problem was that while it is difficult to negate these belief issues, we were not even approaching many of the families because we did not have an effective process that identifies the potential donors in all the hospitals,” says Prof. Barbash. “As a result, we were approaching only half of the families of potential donors.”
To tackle the problem, the Ministry of Health hired a nurse stationed in every Israeli hospital designated to identify candidates for organ donation and to manage these highly sensitive situations. A nurse director at the National Transplantation Center oversees the national operation and ensures that the harvesting process proceeds smoothly after a family's approval.
Prof. Barbash is a graduate of the Hadassah Medical School of the Hebrew University of Jerusalem and is board certified in Internal Medicine, Medical Management, and Occupational Medicine. He holds a master’s degree in public health from the Harvard University School of Public Health. He was Israel’s national coordinator and principal investigator for numerous multi-center cardiology studies (1989-2000). He is a Professor of Epidemiology and Preventive Medicine at Tel Aviv University's Sackler School of Medicine.
He is widely published in his field, cardiology, specifically acute myocardial infarction, and was a visiting professor at Columbia University.
http://compgenomics.weizmann.ac.il/tanay
Prof. Amos Tanay







