Endotoxic shock resulting from exposure to high doses of lipopolysaccharide (LPS), a constituent of the bacterial cell wall, is the most common cause of death in intensive care units. Pioneering work by Halberg in the 1960s showed increased susceptibility in mice injected with E. Coli endotoxin in the noon (till evening) in contrast to mice injected with endotoxin from midnight (till morning). Recent findings have identified molecular mechanisms involved in the circadian regulation of a variety of immune progenitors, such as hematopoietic stem cells, and mature leukocytes, such as macrophages, as well as inflammatory cytokines. These oscillatory rhythms of immune cells and pro-inflammatory mediators, allow the host to anticipate and handle microbial threats more efficiently. However, a comprehensive study on the circadian regulation of neutrophils during inflammation is currently lacking.
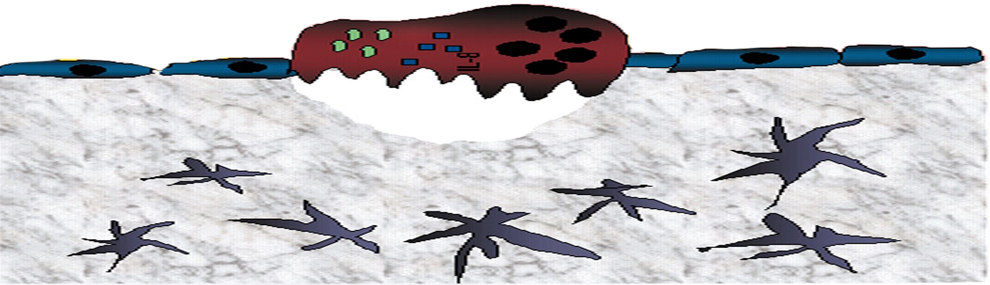
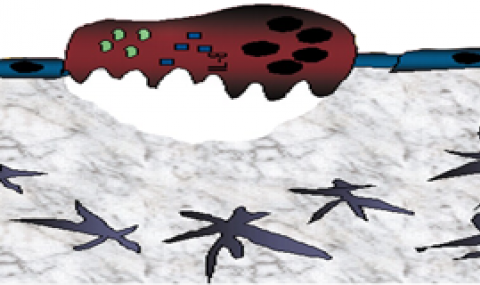
We investigate how the extent of the endotoxin response is regulated by diurnal oscillations in neutrophil phenotype and kinetics. Neutrophils act to resolve infection by phagocytosis, degranulation or the formation of neutrophil extracellular traps (NETs). Our preliminary results reveal that exposure to LPS at different times of the day affects neutrophil differently, leading to variations in neutrophil activation and mobilization. Serine proteases expelled from activated neutrophils bind dense aggregated NETS and play an essential role in degrading cytokines and chemokines, therefore modulating the immune response. Building on these findings, we expect that mice with a poor neutrophil oxidative burst develop an exaggerated inflammatory response to LPS, and subsequently, higher mortality. We aim to provide mechanistic insights into the role of neutrophils and their effector molecules in regulating this process.