Publications
Preprints
2025
The timing of endotoxin administration in mice matters and is associated with diurnal variation in survival; however, underlying mechanisms remain poorly understood. Here, we report that afternoon LPS challenges in mice induce a robust inflammatory response involving increased neutrophil activation and release of cytotoxic mediators, causing higher mortality compared with challenges at midnight. Mechanistically, the cyclic patterns of corticosterone and melatonin hormones differentially modulate neutrophil responses. The afternoon corticosterone peak was associated with heightened incidence and severity of LPS-induced hyperinflammation. Conversely, higher melatonin levels at midnight conferred protection to challenged mice by restraining the magnitude of inflammation. High cortisol and low melatonin profiles detected in septic patients mirror those observed in mice and suggest a novel prognostic marker for sepsis. Our study unveils a regulatory network that links light/dark signals and circadian-regulated hormones to the intensity of the host's inflammatory response to infection.
2024
Summary Classical monocytes (CMs) are ephemeral myeloid immune cells that circulate in the blood. Emerging evidence suggests that CMs can have distinct ontogeny and originate from either granulocyte-monocyte- or monocyte-dendritic-cell progenitors (GMPs or MDPs). Here, we report surface markers that allowed segregation of murine GMP- and MDP-derived CMs, i.e., GMP-Mo and MDP-Mo, as well as their functional characterization, including fate definition following adoptive cell transfer. GMP-Mo and MDP-Mo yielded an equal increase in homeostatic CM progeny, such as blood-resident non-classical monocytes and gut macrophages; however, these cells differentially seeded various other selected tissues, including the dura mater and lung. Specifically, GMP-Mo and MDP-Mo differentiated into distinct interstitial lung macrophages, linking CM dichotomy to previously reported pulmonary macrophage heterogeneity. Collectively, we provide evidence for the existence of two functionally distinct CM subsets in the mouse that differentially contribute to peripheral tissue macrophage populations in homeostasis and following challenge.
2023
2022
In vitro cultured stem cells with distinct developmental capacities can contribute to embryonic or extra-embryonic tissues after microinjection into pre-implantation mammalian embryos. However, whether cultured stem cells can independently give rise to entire gastrulating embryo-like structures with embryonic and extra-embryonic compartments, remains unknown. Here we adapt a recently established platform for prolonged ex utero growth of natural embryos, to generate mouse post-gastrulation synthetic whole embryo models (sEmbryos), with both embryonic and extra-embryonic compartments, starting solely from naïve ESCs. This was achieved by co-aggregating non-transduced ESCs, with naïve ESCs transiently expressing Cdx2- and Gata4- to promote their priming towards trophectoderm and primitive endoderm lineages, respectively. sEmbryos adequately accomplish gastrulation, advance through key developmental milestones, and develop organ progenitors within complex extra-embryonic compartments similar to E8.5 stage mouse embryos. Our findings highlight the plastic potential of naïve pluripotent cells to self-organize and functionally reconstitute and model the entire mammalian embryo beyond gastrulation.
Consecutive exposures to different pathogens are highly prevalent and often alter the host immune response. However, it remains unknown how a secondary bacterial infection affects an ongoing adaptive immune response elicited against primary invading pathogens. We demonstrated that recruitment of Sca-1+ monocytes into lymphoid organs during Salmonella Typhimurium (STm) infection disrupted pre-existing germinal center (GC) reactions. GC responses induced by influenza, plasmodium, or commensals deteriorated following STm infection. GC disruption was independent of the direct bacterial interactions with B cells and instead was induced through recruitment of CCR2-dependent Sca-1+ monocytes into the lymphoid organs. GC collapse was associated with impaired cellular respiration and was dependent on TNFα and IFNγ, the latter of which was essential for Sca-1+ monocyte differentiation. Monocyte recruitment and GC disruption also occurred during LPS-supplemented vaccination and Listeria monocytogenes infection. Thus, systemic activation of the innate immune response upon severe bacterial infection is induced at the expense of antibody-mediated immunity.
Hematopoietic stem cells (HSCs) located at the top of the hematopoietic hierarchy are metabolically and dynamically adjusted to concomitantly generate millions of mature blood and immune cells daily while maintaining the potential of these primitive, bone marrow (BM) retained stem cells to self-renew, to repopulate ablated BM and to reinitiate hematopoiesis following their transplantation. These processes involve dynamic changes in the phenotype and molecular activities of HSCs concerning their localization, adhesion, cell-cycle status, migration, differentiation, metabolic activity, and chemotherapy resistance. Many key players regulating HSC function have been revealed and the dominant role of microenvironmental regulating signals originated in the BM stem cell niches have been recently elucidated. This chapter discusses mechanisms that regulate clinically relevant aspects of human HSC transplantation, namely, homing and mobilization, focusing on the major roles of the CXCL12/CXCR4 axis and the dynamic metabolic control of HSC function.
2021
2020
The fate of hematopoietic stem and progenitor cells (HSPC) is tightly regulated by their bone marrow (BM) microenvironment (ME). BM transplantation (BMT) frequently requires irradiation preconditioning to ablate endogenous hematopoietic cells. Whether the stromal ME is damaged and how it recovers after irradiation is unknown. We report that BM mesenchymal stromal cells (MSC) undergo massive damage to their mitochondrial function after irradiation. Donor healthy HSPC transfer functional mitochondria to the stromal ME, thus improving mitochondria activity in recipient MSC. Mitochondrial transfer to MSC is cell-contact dependent and mediated by HSPC connexin-43 (Cx43). Hematopoietic Cx43-deficient chimeric mice show reduced mitochondria transfer, which was rescued upon re-expression of Cx43 in HSPC or culture with isolated mitochondria from Cx43 deficient HSPCs. Increased intracellular adenosine triphosphate levels activate the purinergic receptor P2RX7 and lead to reduced activity of adenosine 5'-monophosphate-activated protein kinase (AMPK) in HSPC, dramatically increasing mitochondria transfer to BM MSC. Host stromal ME recovery and donor HSPC engraftment were augmented after mitochondria transfer. Deficiency of Cx43 delayed mesenchymal and osteogenic regeneration while in vivo AMPK inhibition increased stromal recovery. As a consequence, the hematopoietic compartment reconstitution was improved because of the recovery of the supportive stromal ME. Our findings demonstrate that healthy donor HSPC not only reconstitute the hematopoietic system after transplantation, but also support and induce the metabolic recovery of their irradiated, damaged ME via mitochondria transfer. Understanding the mechanisms regulating stromal recovery after myeloablative stress are of high clinical interest to optimize BMT procedures and underscore the importance of accessory, non-HSC to accelerate hematopoietic engraftment.
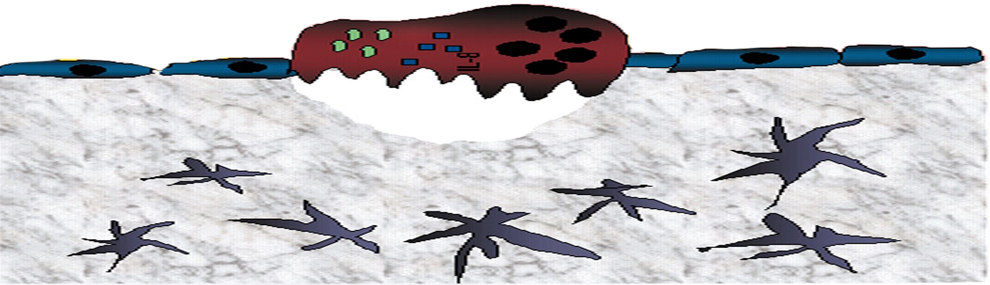
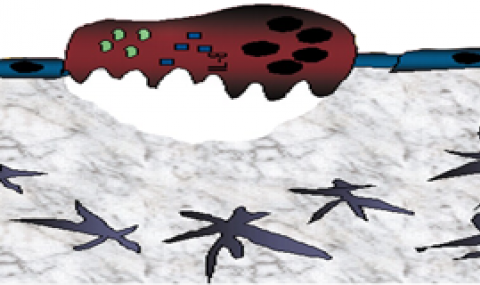
Neutrophils provide first line of host defense against bacterial infections utilizing glycolysis for their effector functions. How glycolysis and its major byproduct lactate are triggered in bone marrow (BM) neutrophils and their contribution to neutrophil mobilization in acute inflammation is not clear. Here we report that bacterial lipopolysaccharides (LPS) or Salmonella Typhimurium triggers lactate release by increasing glycolysis, NADPH-oxidase-mediated reactive oxygen species and HIF-1α levels in BM neutrophils. Increased release of BM lactate preferentially promotes neutrophil mobilization by reducing endothelial VE-Cadherin expression, increasing BM vascular permeability via endothelial lactate-receptor GPR81 signaling. GPR81-/- mice mobilize reduced levels of neutrophils in response to LPS, unless rescued by VE-Cadherin disrupting antibodies. Lactate administration also induces release of the BM neutrophil mobilizers G-CSF, CXCL1 and CXCL2, indicating that this metabolite drives neutrophil mobilization via multiple pathways. Our study reveals a metabolic crosstalk between lactate-producing neutrophils and BM endothelium, which controls neutrophil mobilization under bacterial infection.
2019
Hematopoietic stem and progenitor cells (HSPCs) are essential for daily mature blood cell production, host immunity, and osteoclast-mediated bone turnover. The timing at which stem cells give rise to mature blood and immune cells while maintaining the bone marrow (BM) reservoir of undifferentiated HSPCs and how these opposite tasks are synchronized are poorly understood. Previous studies revealed that daily light onset activates norepinephrine (NE)-induced BM CXCL12 downregulation, followed by CXCR4+ HSPC release to the circulation. Recently, we reported that daily light onset induces transient elevations of BM NE and tumor necrosis factor (TNF), which metabolically program BM HSPC differentiation and recruitment to replenish the blood. In contrast, darkness onset induces lower elevations of BM NE and TNF, activating melatonin production, which metabolically reprograms HSPCs, increasing their short- and long-term repopulation potential, and BM maintenance. How the functions of BM-retained HSPCs are influenced by daily light and darkness cycles and their clinical potential are further discussed.
Hematopoietic stem cell transplantation has been established as a curative treatment for patients with hematological malignancies. Understanding the regulation of Hematopoietic Stem and Progenitor Cells (HSPC) is crucial to improve the outcomes of transplants. Others and we have previously shown the role of coagulation-linked pathways in regulation of murine HSPC egress and retention. Particularly, different activities of the major receptor for thrombin, Protease Activated Receptor 1 (PAR1), direct mouse HSPC mobilization versus bone marrow (BM)-retention, driven by thrombin or aPC/EPCR cleavage, respectively. Acute stress and clinical mobilization, upregulate thrombin generation, which cleaves PAR1 to activate pro-inflammatory signaling, inducing HSPC recruitment to the bloodstream. PAR1 can alternatively interact with Endothelial Protein Receptor C (EPCR) activating anti-inflammatory signaling, to retain long term repopulating HSPC in the BM by restricting nitric oxide (NO) generation.1,2 These studies investigated the role of coagulation-related pathways only in experimental mouse models and their relevance to clinical protocols is currently unknown.
2018
Hematopoietic stem and progenitor cells (HSPCs) tightly couple maintenance of the bone marrow (BM) reservoir, including undifferentiated long-term repopulating hematopoietic stem cells (LT-HSCs), with intensive daily production of mature leukocytes and blood replenishment. We found two daily peaks of BM HSPC activity that are initiated by onset of light and darkness providing this coupling. Both peaks follow transient elevation of BM norepinephrine and TNF secretion, which temporarily increase HSPC reactive oxygen species (ROS) levels. Light-induced norepinephrine and TNF secretion augments HSPC differentiation and increases vascular permeability to replenish the blood. In contrast, darkness-induced TNF increases melatonin secretion to drive renewal of HSPCs and LT-HSC potential through modulating surface CD150 and c-Kit expression, increasing COX-2/αSMA
+ macrophages, diminishing vascular permeability, and reducing HSPC ROS levels. These findings reveal that light- and darkness-induced daily bursts of norepinephrine, TNF, and melatonin within the BM are essential for synchronized mature blood cell production and HSPC pool repopulation. Golan et al. report that daily onsets of light and dark induce NE and TNF bursts that induce two different peaks of BM HSPC activity. Light-induced NE promotes HSPC differentiation and egress, replenishing mature blood cells. Dark-induced TNF promotes melatonin-dependent renewal of CD150
+ HSCs and their long-term repopulation potential.
The hemostatic system plays pivotal roles in injury repair, innate immunity, and adaptation to inflammatory challenges. We review the evidence that these vascular-protective mechanisms have nontraditional roles in hematopoietic stem cell (HSC) maintenance in their physiological bone marrow (BM) niches at steady-state and under stress. Expression of coagulation factors and the extrinsic coagulation initiator tissue factor by osteoblasts, tissue-resident macrophages, and megakaryocytes suggests that endosteal and vascular HSC niches are functionally regulated by extravascular coagulation. The anticoagulant endothelial protein C receptor (EPCR; Procr) is highly expressed by primitive BM HSCs and endothelial cells. EPCR is associated with its major ligand, activated protein C (aPC), in proximity to thrombomodulin-positive blood vessels, enforcing HSC integrin alpha 4 adhesion and chemotherapy resistance in the context of CXCL12-CXCR4 niche retention signals. Protease-activated receptor 1-biased signaling by EPCR-aPC also maintains HSC retention, whereas thrombin signaling activates HSC motility and BM egress. Furthermore, HSC mobilization under stress is enhanced by the fibrinolytic and complement cascades that target HSCs and their BM niches. In addition, coagulation, fibrinolysis, and HSC-derived progeny, including megakaryocytes, synergize to reestablish functional perivascular HSC niches during BM stress. Therapeutic restoration of the anticoagulant pathway has preclinical efficacy in reversing BM failure following radiation injury, but questions remain about how antithrombotic therapy influences extravascular coagulation in HSC maintenance and hematopoiesis.
2017
2016
Generation and growth of the blood vasculature network is a highly synchronized process, requiring coordinated efforts of endothelial cells and pericytes to maintain blood vessel integrity and regeneration. In a recent paper published in Cell Research, Yu et al. identified and characterized bipotent Procr-expressing vascular endothelial stem cells, which give rise to both endothelial cells and pericytes.
In addition to their conventional role as a versatile transport system, blood vessels provide signals controlling organ development, regeneration, and stem cell behavior. In the skeletal system, certain capillaries support perivascular osteoprogenitor cells and thereby control bone formation. Blood vessels are also a critical component of niche microenvironments for hematopoietic stem cells. Here we discuss key pathways and factors controlling endothelial cell behavior in bone, the role of vessels in osteogenesis, and the nature of vascular stem cell niches in bone marrow.
The common developmental origin of endothelial and hematopoietic cells is manifested by coexpression of several cell surface receptors. Adultmurine bonemarrow (BM) long-term repopulating hematopoietic stem cells (LT-HSCs), endowed with the highest repopulation and self-renewal potential, express endothelial protein C receptor (EPCR), which is used as a marker to isolate them. EPCR/protease-activated receptor-1 (PAR1) signaling in endothelial cells has anticoagulant and anti-inflammatory roles, while thrombin/PAR1 signaling induces coagulation and inflammation. Recent studies define two new PAR1-mediated signaling cascades that regulate EPCR+ LT-HSC BM retention and egress. EPCR/PAR1 signaling facilitates LT-HSC BM repopulation, retention, survival, and chemotherapy resistance by restricting nitric oxide (NO) production, maintaining NOlow LT-HSC BM retention with increased VLA4 expression, affinity, and adhesion. Conversely, acute stress and clinical mobilization upregulate thrombin generation and activate different PAR1 signaling that overcomes BM EPCR+ LT-HSC retention, inducing their recruitment to the bloodstream. Thrombin/PAR1 signaling induces NO generation, TACE-mediated EPCR shedding, and upregulation of CXCR4 and PAR1, leading to CXCL12-mediated stem and progenitor cell mobilization. This review discusses new roles for factors traditionally viewed as coagulation related, which independently act in the BM to regulate PAR1 signaling in bone-and blood-forming progenitor cells, navigating their fate by controlling NO production.
Blood vessels define local microenvironments in the skeletal system, play crucial roles in osteogenesis and provide niches for haematopoietic stem cells. The properties of niche-forming vessels and their changes in the ageing organism remain incompletely understood. Here we show that Notch signalling in endothelial cells leads to the expansion of haematopoietic stem cell niches in bone, which involves increases in CD31-positive capillaries and platelet-derived growth factor receptor-β (PDGFRβ)-positive perivascular cells, arteriole formation and elevated levels of cellular stem cell factor. Although endothelial hypoxia-inducible factor signalling promotes some of these changes, it fails to enhance vascular niche function because of a lack of arterialization and expansion of PDGFRβ-positive cells. In ageing mice, niche-forming vessels in the skeletal system are strongly reduced but can be restored by activation of endothelial Notch signalling. These findings indicate that vascular niches for haematopoietic stem cells are part of complex, age-dependent microenvironments involving multiple cell populations and vessel subtypes.
Bone marrow endothelial cells (BMECs) form a network of blood vessels that regulate both leukocyte trafficking and haematopoietic stem and progenitor cell (HSPC) maintenance. However, it is not clear how BMECs balance these dual roles, and whether these events occur at the same vascular site. We found that mammalian bone marrow stem cell maintenance and leukocyte trafficking are regulated by distinct blood vessel types with different permeability properties. Less permeable arterial blood vessels maintain haematopoietic stem cells in a low reactive oxygen species (ROS) state, whereas the more permeable sinusoids promote HSPC activation and are the exclusive site for immature and mature leukocyte trafficking to and from the bone marrow. A functional consequence of high permeability of blood vessels is that exposure to blood plasma increases bone marrow HSPC ROS levels, augmenting their migration and differentiation, while compromising their long-term repopulation and survival. These findings may have relevance for clinical haematopoietic stem cell transplantation and mobilization protocols.
2015
Retention of long-term repopulating hematopoietic stem cells (LT-HSCs) in the bone marrow is essential for hematopoiesis and for protection from myelotoxic injury. We report that signaling cascades that are traditionally viewed as coagulation related also control retention of endothelial protein C receptor-positive (EPCR +) LT-HSCs in the bone marrow and their recruitment to the blood via two pathways mediated by protease activated receptor 1 (PAR1). Thrombin-PAR1 signaling induces nitric oxide (NO) production, leading to EPCR shedding mediated by tumor necrosis factor-α-converting enzyme (TACE), enhanced CXCL12-CXCR4-induced motility and rapid stem and progenitor cell mobilization. Conversely, bone marrow blood vessels provide a microenvironment enriched with activated protein C (aPC) that retains EPCR + LT-HSCs by limiting NO generation, reducing Cdc42 activity and enhancing integrin VLA4 affinity and adhesion. Inhibition of NO production by aPC-EPCR-PAR1 signaling reduces progenitor cell egress from the bone marrow, increases retention of bone marrow NO low EPCR + LT-HSCs and protects mice from chemotherapy-induced hematological failure and death. Our study reveals new roles for PAR1 and EPCR in controlling NO production to balance maintenance and recruitment of bone marrow EPCR + LT-HSCs, with potential clinical relevance for stem cell transplantation.
Amplified HER2, which encodes a member of the epidermal growth factor receptor (EGFR) family, is a target of effective therapies against breast cancer. In search for similarly targetable genomic aberrations, we identified copy number gains in SYNJ2, which encodes the 5-inositol lipid phosphatase synaptojanin 2, as well as overexpression in a small fraction of human breast tumors. Copy gain and overexpression correlated with shorter patient survival and a low abundance of the tumor suppressor microRNA miR-31. SYNJ2 promoted cell migration and invasion in culture and lung metastasis of breast tumor xenografts in mice. Knocking down SYNJ2 impaired the endocytic recycling of EGFR and the formation of cellular lamellipodia and invadopodia. Screening compound libraries identified SYNJ2-specific inhibitors that prevented cell migration but did not affect the related neural protein SYNJ1, suggesting that SYNJ2 is a potentially druggable target to block cancer cell migration.
2014
Significance: Blood forming, hematopoietic stem cells (HSCs) mostly reside in the bone marrow in a quiescent, nonmotile state via adhesion interactions with stromal cells and macrophages. Quiescent, proliferating, and differentiating stem cells have different metabolism, and accordingly different amounts of intracellular reactive oxygen species (ROS). Importantly, ROS is not just a byproduct of metabolism, but also plays a role in stem cell state and function. Recent Advances: ROS levels are dynamic and reversibly dictate enhanced cycling and myeloid bias in ROShighshort-term repopulating stem cells, and ROSlowquiescent long-term repopulating stem cells. Low levels of ROS, regulated by intrinsic factors such as cell respiration or nicotinamide adenine dinucleotide phosphate-oxidase (NADPH oxidase) activity, or extrinsic factors such as stem cell factor or prostaglandin E2 are required for maintaining stem cell self-renewal. High ROS levels, due to stress and inflammation, induce stem cell differentiation and enhanced motility. Critical Issues: Stem cells need to be protected from high ROS levels to avoid stem cell exhaustion, insufficient host immunity, and leukemic transformation that may occur during chronic inflammation. However, continuous low ROS production will lead to lack of stem cell function and opportunistic infections. Ultimately, balanced ROS levels are crucial for maintaining the small stem cell pool and host immunity, both in homeostasis and during stress situations. Future Directions: Deciphering the signaling pathway of ROS in HSC will provide a better understanding of ROS roles in switching HSC from quiescence to activation and vice versa, and will also shed light on the possible roles of ROS in leukemia initiation and development. Antioxid. Redox Signal. 21, 1605-1619.
2013
The role of corticosterone (Cort), the immune system's major stress hormone, in the regulation of hematopoietic stem and progenitor cells (HSPCs) and their dynamic bone marrow (BM) microenvironment is currently unknown. We report that corticotropin-releasing factor receptor 1 (CRFR1) mutant mice with chronically low Cort levels showed aberrant HSPC regulation, having higher HSPC numbers and upregulation of the chemokine CXCL12, phenotypes that were restored by Cort supplementation. Expanded stromal progenitors known to support HSPCs were also observed in these low-Cort-containing mice. A similar phenotype was induced in wild-type (WT) mice by Metyrapone, a Cort synthesis inhibitor. Conversely, high Cort exposure induced HSPC apoptosis, reduced long-term BM repopulation and decreased stromal progenitor cell numbers. We documented circadian oscillations of Cort in WT BM but not in CRFR1 mutant mice, leading to diminished circadian BM CXCL12 fluctuations and increased number of circulating HSPCs in these mice. Finally, low Cort induced expansion of stromal progenitors, CXCL12 expression, HSPC proliferation and BM repopulation capacity, involving Notch1 signaling. This was associated with upregulation of the Notch ligand, Jagged1, in BM myeloid cells. Our results suggest that daily physiologic Cort oscillations are critical for balanced HSPC proliferation and function involving Notch1 signaling and their supportive BM microenvironment.
Hematopoietic stem cells (HSCs) are mostly retained in a quiescent non-motile mode in their bone marrow (BM) niches, shifting to a migratory cycling and differentiating state to replenish the blood with mature leukocytes on demand. The balance between the major chemo-attractants CXCL12, predominantly in the BM, and S1P, mainly in the blood, dynamically regulates HSC recruitment to the circulation versus their retention in the BM. During alarm situations, stress-signals induce a decrease in CXCL12 levels in the BM, while S1P levels are rapidly and transiently increased in the circulation, thus favoring mobilization of stem cells as part of host defense and repair mechanisms. Myeloid cytokines, including G-CSF, up-regulate S1P signaling in the BM via the PI3K pathway. Induced CXCL12 secretion from stromal cells via reactive oxygen species (ROS) generation and increased S1P1 expression and ROS signaling in HSCs, all facilitate mobilization. Bone turnover is also modulated by both CXCL12 and S1P, regulating the dynamic BM stromal microenvironment, osteoclasts and stem cell niches which all functionally express CXCL12 and S1P receptors. Overall, CXCL12 and S1P levels in the BM and circulation are synchronized to mutually control HSC motility, leukocyte production and osteoclast/osteoblast bone turnover during homeostasis and stress situations.
Purpose of Review: Fibroblast growth factor (FGF) signaling activates many bone marrow cell types, including various stem cells, osteoblasts, and osteoclasts. However, the role of FGF signaling in regulation of normal and leukemic stem cells is poorly understood. This review highlights the physiological roles of FGF signaling in regulating bone marrow mesenchymal and hematopoietic stem and progenitor cells (MSPCs and HSPCs) and their dynamic microenvironment. In addition, this review summarizes the recent studies which provide an overview of FGF-activated mechanisms regulating physiological stem cell maintenance, self-renewal, and motility. Recent Findings: Current results indicate that partial deficiencies in FGF signaling lead to mild defects in hematopoiesis and bone remodeling. However, FGF signaling was shown to be crucial for stem cell self-renewal and for proper hematopoietic poststress recovery. FGF signaling activation was shown to be important also for rapid AMD3100 or post 5-fluorouracil-induced HSPC mobilization. In vivo, FGF-2 administration successfully expanded both MSPCs and HSPCs. FGF-induced expansion was characterized by enhanced HSPC cycling without further exhaustion of the stem cell pool. In addition, FGF signaling expands and remodels the supportive MSPC niche cells. Finally, FGF signaling is constitutively activated in many leukemias, suggesting that malignant HSPCs exploit this pathway for their constant expansion and for remodeling a malignant-supportive microenvironment. Summary: The summarized studies, concerning regulation of stem cells and their microenvironment, suggest that FGF signaling manipulation can serve to improve current clinical stem cell mobilization and transplantation protocols. In addition, it may help to develop therapies specifically targeting leukemic stem cells and their supportive microenvironment.
Regulation of hematopoietic stem and progenitor cell (HSPC) steady-state egress from the bone marrow (BM) to the circulation is poorly understood. While glycogen synthase kinase-3β (GSK3β) is known to participate in HSPC proliferation, we revealed an unexpected role in the preferential regulation of CXCL12-induced migration and steady-state egress of murine HSPCs, including long-term repopulating HSCs, over mature leukocytes. HSPC egress, regulated by circadian rhythms of CXCL12 and CXCR4 levels, correlated with dynamic expression of GSK3β in the BM. Nevertheless, GSK3β signaling was CXCL12/CXCR4 independent, suggesting that synchronization of both pathways is required for HSPC motility. Chemotaxis of HSPCs expressing higher levels of GSK3β compared with mature cells was selectively enhanced by stem cell factor-induced activation of GSK3β. Moreover, HSPC motility was regulated by norepinephrine and insulin-like growth factor-1 (IGF-1), which increased or reduced, respectively, GSK3β expression in BM HSPCs and their subsequent egress. Mechanistically, GSK3β signaling promoted preferential HSPC migration by regulating actin rearrangement and microtubuli turnover, including CXCL12-induced actin polarization and polymerization. Our study identifies a previously unknown role for GSK3β in physiological HSPC motility, dictating an active, rather than a passive, nature for homeostatic egress from the BM reservoir to the blood circulation.
2012
Hematopoietic stem and progenitor cells (HSPCs) are regulated by various bone marrow stromal cell types. Here we identified rare activated bone marrow monocytes and macrophages with high expression of α-smooth muscle actin (α-SMA) and the cyclooxygenase COX-2 that were adjacent to primitive HSPCs. These myeloid cells resisted radiation-induced cell death and further upregulated COX-2 expression under stress conditions. COX-2-derived prostaglandin E 2 (PGE 2) prevented HSPC exhaustion by limiting the production of reactive oxygen species (ROS) via inhibition of the kinase Akt and higher stromal-cell expression of the chemokine CXCL12, which is essential for stem-cell quiescence. Our study identifies a previously unknown subset of α-SMA + activated monocytes and macrophages that maintain HSPCs and protect them from exhaustion during alarm situations.
The cancer stem cell (CSC) concept has important therapeutic implications, but its investigation has been hampered both by a lack of consistency in the terms used for these cells and by how they are defined. Evidence of their heterogeneous origins, frequencies and their genomic, as well as their phenotypic and functional, properties has added to the confusion and has fuelled new ideas and controversies. Participants in The Year 2011 Working Conference on CSCs met to review these issues and to propose a conceptual and practical framework for CSC terminology. More precise reporting of the parameters that are used to identify CSCs and to attribute responses to them is also recommended as key to accelerating an understanding of their biology and developing more effective methods for their eradication in patients.
Cytokine-induced expansion of hematopoietic stem and progenitor cells (HSPCs) is not fully understood. In the present study, we show that whereas steady-state hematopoiesis is normal in basic fibroblast growth factor (FGF-2)-knockout mice, parathyroid hormone stimulation and myeloablative treatments failed to induce normal HSPC proliferation and recovery. In vivo FGF-2 treatment expanded stromal cells, including perivascular Nestin + supportive stromal cells, which may facilitate HSPC expansion by increasing SCF and reducing CXCL12 via mir-31 up-regulation. FGF-2 predominantly expanded a heterogeneous population of undifferentiated HSPCs, preserving and increasing durable short- and long-term repopulation potential. Mechanistically, these effects were mediated by c-Kit receptor activation, STAT5 phosphorylation, and reduction of reactive oxygen species levels. Mice harboring defective c-Kit signaling exhibited abrogated HSPC expansion in response to FGF-2 treatment, which was accompanied by elevated reactive oxygen species levels. The results of the present study reveal a novel mechanism underlying FGF-2-mediated in vivo expansion of both HSPCs and their supportive stromal cells, which may be used to improve stem cell engraftment after clinical transplantation.
Previous studies have shown that fibroblast growth factor (FGF) signaling promotes hematopoietic stem and progenitor cell (HSPC) expansion in vitro. However, it is unknown whether FGF promotes HSPC expansion in vivo. Here we examined FGF receptor 1 (FGFR1) expression and investigated its in vivo function in HSPCs. Conditional knockout (CKO) of Fgfr1 did not affect phenotypical number of HSPCs and homeostatic hematopoiesis, but led to a reduced engraftment only in the secondary transplantation. When treated with 5-fluorouracil (5FU), the Fgfr1 CKO mice showed defects in both proliferation and subsequent mobilization of HSPCs. We identified megakaryocytes (Mks) as a major resource for FGF production, and further discovered a novel mechanism by which Mks underwent FGF-FGFR signaling dependent expansion to accelerate rapid FGF production under stress. Within HSPCs, we observed an up-regulation of nuclear factor κB and CXCR4, a receptor for the chemoattractant SDF-1, in response to bone marrow damage only in control but not in Fgfr1 CKO model, accounting for the corresponding defects in proliferation and migration of HSPCs. This study provides the first in vivo evidence that FGF signaling facilitates postinjury recovery of the mouse hematopoietic system by promoting proliferation and facilitating mobilization of HSPCs.
Allogeneic donor blood cells and autologous peripheral blood leukocytes (PBL), obtained following clinical mobilization procedures, are routinely used as a major source of hematopoietic stem and progenitor cells (HSPC) for transplantation protocols. It is, therefore, essential to evaluate and to quantify the extent by which the HSPC are mobilized and enriched in the circulation in correlation with their long-term hematopoietic reconstitution capacity. In this chapter, we describe quantitative methods that measure the number of mobilized HSPC according to specific criteria, as well as their functional properties in vitro and in vivo. The described assays are useful for assessment of progenitor cell mobilization as applied to both human and murine HSPC.
BID, a BH3-only BCL2 family member, functions in apoptosis as well as the DNA-damage response. Our previous data demonstrated that BID is an ATM effector acting to induce cell-cycle arrest and inhibition of apoptosis following DNA damage. Here we show that ATM-mediated BID phosphorylation plays an unexpected role in maintaining the quiescence of haematopoietic stem cells (HSCs). Loss of BID phosphorylation leads to escape from quiescence of HSCs, resulting in exhaustion of the HSC pool and a marked reduction of HSC repopulating potential in vivo. We also demonstrate that BID phosphorylation plays a role in protecting HSCs from irradiation, and that regulating both quiescence and survival of HSCs depends on BID's ability to regulate oxidative stress. Moreover, loss of BID phosphorylation, ATM knockout or exposing mice to irradiation leads to an increase in mitochondrial BID, which correlates with an increase in mitochondrial oxidative stress. These results show that the ATM-BID pathway serves as a critical checkpoint for coupling HSC homeostasis and the DNA-damage stress response to enable long-term regenerative capacity.
The mechanisms of hematopoietic progenitor cell egress and clinical mobilization are not fully understood. Herein, we report that in vivo desensitization of Sphingosine-1-phosphate (S1P) receptors by FTY720 as well as disruption of S1P gradient toward the blood, reduced steady state egress of immature progenitors and primitive Sca-1+/c-Kit+/Lin - (SKL) cells via inhibition of SDF-1 release. Administration of AMD3100 or G-CSF to mice with deficiencies in either S1P production or its receptor S1P1, or pretreated with FTY720, also resulted in reduced stem and progenitor cell mobilization. Mice injected with AMD3100 or G-CSF demonstrated transient increased S1P levels in the blood mediated via mTOR signaling, as well as an elevated rate of immature c-Kit+/Lin - cells expressing surface S1P1 in the bone marrow (BM). Importantly, we found that S1P induced SDF-1 secretion from BM stromal cells including Nestin+ mesenchymal stem cells via reactive oxygen species (ROS) signaling. Moreover, elevated ROS production by hematopoietic progenitor cells is also regulated by S1P. Our findings reveal that the S1P/S1P1 axis regulates progenitor cell egress and mobilization via activation of ROS signaling on both hematopoietic progenitors and BM stromal cells, and SDF-1 release. The dynamic cross-talk between S1P and SDF-1 integrates BM stromal cells and hematopoeitic progenitor cell motility.
Egress and Mobilization of Hematopoietic Stem and Progenitor Cells: A dynamic multi-facet process
Adult hematopoietic stem cells (HSC) continuously replenish the blood with immune and blood cells with a finite life span, from the bone marrow (BM) reservoir of immature and maturing leukocytes. Regulation of HSC migration and development is essential for their function and blood cell production. These diverse and multiple states require a tight regulation to efficiently address host defense and repair requirements. Numerous recent studies disclose a central role for bone related cells in regulation of HSC and hematopoiesis. During ontogeny HSC home and seed the fetal BM in the last gestation period when the bone is already ossified. Ossification involves bone forming osteoblast- and bone degrading osteoclast activity and is considered essential for the formation of BM cavities and hematopoiesis. This synchronized association implies the need for active bone cells and bone turnover for HSC regulation. Osteoblastic cells and SDF-1+/nestin+ reticular adventitial and CAR cells are crucial for regulation of HSC lodgment, self-renewal and function. Bone resorbing osteoclasts regulate bone turnover and progenitor cell detachment and release from the BM. Sympathetic signals from the nervous system activated by circadian rhythms or stress conditions control both bone turnover and HSC migration and development. In this review we discuss pathways and mechanisms involved in this orchestrated regulatory network. A special focus is made on the pivotal role of the SDF-1/CXCR4 axis as a determinant of HSC fate. Inflammation, DNA damage, cytokine mobilization, microgravity and aging are discussed as specific physiologic and pathologic events entailing dysregulation of the tightly balanced Bone-Brain-Blood triad.
2011
Migratory capacity is a fundamental property of hematopoietic stem and progenitor cells (HSPCs). This feature is employed in clinical mobilization of HSPCs to the circulation and constitutes the basis for modern bone marrow (BM) transplantation procedures which are routinely used to treat hematological malignancies. Therefore, characterization of new players in the complex process of HSPC motility in steady-state conditions as well as during stress situations is a major challenge. We report that while the metalloproteinase membrane type 1-metalloprotease (MT1-MMP) has an essential role in human HSPC trafficking during granulocyte colony-stimulating factor (G-CSF)-induced mobilization, its inhibitor reversion-inducing cysteine-rich protein with Kazal motifs (RECK) and the adhesion molecule CD44 are required for HSPC retention to the BM in steady-state conditions. The nervous system via Wnt signaling along with HGF/c-Met signaling and the complement cascade play a major role in regulating MT1-MMP increased activity, CD44 cleavage, and RECK-reduced expression during G-CSF-induced mobilization. This review will elaborate on the opposite roles of MT1-MMP and RECK in HSPC migration and retention and suggest targeting them in order to facilitate HSPC mobilization and engraftment upon BM transplantation in patients.
Bone marrow homing and engraftment by clinically transplanted hematopoietic stem and progenitor cells is a complex process that is not fully understood. We report that the pan-leukocyte CD45 phosphatase plays an essential role in trafficking and repopulation of the bone marrow by immature human CD34+ cells and leukemic cells in transplanted nonobese diabetic severe combined immunodeficient mice. Inhibiting CD45 function by blocking antibodies or a CD45 inhibitor impaired the motility of both normal and leukemic human cells. Blocking CD45 inhibited homing and repopulation by immature human CD34+ cells as well as homing of primary patient leukemic cells. In addition, CD45 inhibition negatively affected development of hematopoietic progenitors in vitro and their recovery in transplanted recipients in vivo, revealing the central role of CD45 in the regulation of hematopoiesis. Moreover, CD45 blockage induced a hyperadhesive phenotype in immature human progenitor cells as well as in murine leukocytes, leading to their defective adhesion interactions with endothelial cells. This phenotype was further manifested by the ability of CD45 blockage to prevent breakdown of adhesion interactions in the BM, which inhibited murine progenitor mobilization. The substantial effects of a direct CD45 inhibition point at its essential roles in cell trafficking, including murine progenitor cell mobilization and both normal immature and leukemic human hematopoietic cells as well as regulation of hematopoiesis and engraftment potential.
Mobilization of hematopoietic stem and progenitor cells (HSPCs) from the bone marrow to the peripheral blood is utilized in clinical HSPC transplantation protocols. Retention of HSPCs in the bone marrow is determined by relationships between the chemokine chemokine (C-X-C motif) ligand 12 (CXCL12) and its major receptor C-X-C chemokine receptor type 4 (CXCR4), and disruption of this retention by CXCR4 antagonists such as AMD3100 induces rapid HSPC mobilization. Here, we report that aminoglycoside-polyarginine conjugates (APACs) and N-α-acetyl-nona-d-arginine (r9) induce mobilization of white blood cells and, preferentially, immature hematopoietic progenitor cells (HPCs) in mice, similarly to AMD3100. Remarkably, administration of AMD3100 with each one of the APACs or r9 caused additional HPC mobilization. The mobilizing activity of APACs and r9 was accompanied by a significant elevation in plasma CXCL12 levels. To further understand how APACs, r9 and their combinations with AMD3100 compete with CXCL12 binding to CXCR4, as well with antibody against CXCR4 for CXCR4 binding, we have undertaken an approach combining experimental validation and docking to determine plausible binding modes for these ligands. On the basis of our biological and docking findings, and recently published NMR data, we suggest that combination of pairs of compounds such as APACs (or r9) with AMD3100 induces more efficient disruption of the CXCL12-CXCR4 interaction than AMD3100 alone, resulting in enhanced HPC mobilization. Mobilization of hematopoietic stem and progenitor cells (HSPCs) from the bone marrow to the peripheral blood is utilized in clinical HSPC transplantation protocols. Aminoglycoside- polyarginine conjugates (APACs) induce mobilization of white blood cells and preferentially immature hematopoietic progenitor cells in mice. Administration of AMD3100 with each one of the APACs revealed additional HPC mobilization, accompanied by a significant elevation in plasma CXCL12 levels
Steady-state egress of hematopoietic progenitor cells can be rapidly amplified by mobilizing agents such as AMD3100, the mechanism, however, is poorly understood. We report that AMD3100 increased the homeostatic release of the chemokine stromal cell derived factor-1 (SDF-1) to the circulation in mice and non-human primates. Neutralizing antibodies against CXCR4 or SDF-1 inhibited both steady state and AMD3100-induced SDF-1 release and reduced egress of murine progenitor cells over mature leukocytes. Intra-bone injection of biotinylated SDF-1 also enhanced release of this chemokine and murine progenitor cell mobilization. AMD3100 directly induced SDF-1 release from CXCR4 + human bone marrow osteoblasts and endothelial cells and activated uPA in a CXCR4/JNK-dependent manner. Additionally, ROS inhibition reduced AMD3100-induced SDF-1 release, activation of circulating uPA and mobilization of progenitor cells. Norepinephrine treatment, mimicking acute stress, rapidly increased SDF-1 release and progenitor cell mobilization, whereas β2-adrenergic antagonist inhibited both steady state and AMD3100-induced SDF-1 release and progenitor cell mobilization in mice. In conclusion, this study reveals that SDF-1 release from bone marrow stromal cells to the circulation emerges as a pivotal mechanism essential for steady-state egress and rapid mobilization of hematopoietic progenitor cells, but not mature leukocytes.
The hematopoietic stem cell (HSC) is the prototype organ-regenerating stem cell (SC), and by far the most studied type of SC in the body. Currently, HSC-based therapy is the only routinely used SC therapy; however, advances in the field of embryonic SCs and induced pluripotent SCs may change this situation. Interest into in vitro generation of HSCs, including signals for HSC expansion and differentiation from these more primitive SCs, as well as advances in other organ-specific SCs, in particular the intestine, provide promising new applications for SC therapies. Here, we review the basic principles of different SC systems, and on the basis of the experience with HSC-based SC therapy, provide recommendations for clinical application of emerging SC technologies.
The chemokine CXCL12 is essential for the function of hematopoietic stem and progenitor cells. Here we report that secretion of functional CXCL12 from human bone marrow stromal cells (BMSCs) was a cell contact-dependent event mediated by connexin-43 (Cx43) and Cx45 gap junctions. Inhibition of connexin gap junctions impaired the secretion of CXCL12 and homing of leukocytes to mouse bone marrow. Purified human CD34 + progenitor cells did not adhere to noncontacting BMSCs, which led to a much smaller pool of immature cells. Calcium conduction activated signaling by cAMP-protein kinase A (PKA) and induced CXCL12 secretion mediated by the GTPase RalA. Cx43 and Cx45 additionally controlled Cxcl12 transcription by regulating the nuclear localization of the transcription factor Sp1. We suggest that BMSCs form a dynamic syncytium via connexin gap junctions that regulates CXC12 secretion and the homeostasis of hematopoietic stem cells.
Aging is associated with a decline in B-lymphopoiesis in the bone marrow and accumulation of long-lived B cells in the periphery. These changes decrease the body's ability to mount protective antibody responses. We show here that age-related changes in the B lineage are mediated by the accumulating long-lived B cells. Thus, depletion of B cells in old mice was followed by expansion of multipotent primitive progenitors and common lymphoid progenitors, a revival of B-lymphopoiesis in the bone marrow, and generation of a rejuvenated peripheral compartment that enhanced the animal's immune responsiveness to antigenic stimulation. Collectively, our results suggest that immunosenescence in the Blineage is not irreversible and that depletion of the long-lived B cells in old mice rejuvenates the B-lineage and enhances immune competence.
Mechanisms governing stress-induced hematopoietic progenitor cell mobilization are not fully deciphered. We report that during granulocyte colony-stimulating factor-induced mobilization c-Met expression and signaling are up-regulated on immature bone marrow progenitors. Interestingly, stromal cell-derived factor 1/CXC chemokine receptor-4 signaling induced hepatocyte growth factor production and c-Met activation. We found that c-Met inhibition reduced mobilization of both immature progenitors and the more primitive Sca-1+/c-Kit+/Lin- cells and interfered with their enhanced chemotactic migration to stromal cell-derived factor 1. c-Met activation resulted in cellular accumulation of reactive oxygen species by mammalian target of rapamycin inhibition of Forkhead Box, subclass O3a. Blockage of mammalian target of rapamycin inhibition or reactive oxygen species signaling impaired c-Met-mediated mobilization. Our data show dynamic c-Met expression and function in the bone marrow and show that enhanced c-Met signaling is crucial to facilitate stress-induced mobilization of progenitor cells as part of host defense and repair mechanisms.
In this issue of Blood, Tzeng et al report on the generation of adult, conditional SDF-1-deficient mice in which HSC quiescence and endosteal niche localization are impaired.1 (Figure Presented).
Bone marrow niches are specialized microenvironments comprising a heterogeneous population of cells that support and regulate hematopoietic stem and progenitor cells. Considerable advances made in the field of hematopoiesis reveal a cross talk between cells, cytokines and neurotransmitters of the hematopoietic, immune and skeletal systems. Dynamic modulation and regulation of stem cells and their niches in response to internal and external stimuli are essential for homeostasis, host defense and repair. This review presents evidence to substantiate stem cell regulation via the "brain-bone-blood triad" beginning at the embryonic stage and continuing to adulthood.
2010
Navigation of transplanted stem cells to their target organs is essential for clinical bone marrow reconstitution. Recent studies have established that hematopoietic stem cells (HSCs) dynamically change their features and location, shifting from quiescent and stationary cells anchored in the bone marrow to cycling and motile cells entering the circulation. These changes are driven by stress signals. Bidirectional migrations to and from the bone marrow are active processes that form the basis for HSC transplantation protocols. However, how and why HSCs enter and exit the bone marrow as part of host defense and repair is not fully understood. The development of functional, preclinical, immune-deficient NOD/SCID (non-obese diabetic-severe combined immunodeficiency) mice transplantation models has enabled the characterization of normal and leukemic human HSCs and investigation of their biology. Intensive research has revealed multiple tasks for the chemokine SDF-1 (stromal cell-derived factor-1, also known as CXCL12) in HSC interactions with the microenvironment, as well as the existence of overlapping mechanisms controlling stress-induced mobilization and enhanced HSC homing, sequential events of major physiological relevance. These processes entail dynamically interacting, multi-system aspects that link the bone marrow vasculature and stromal cells with the nervous and immune systems. Neural cues act as an external pacemaker to synchronize HSC migration and development to balance bone remodeling via circadian rhythms in order to address blood and immune cell production for the physiological needs of the body. Stress situations and clinical HSC mobilization accelerate leukocyte proliferation and bone turnover. This review presents the concept that HSC regulation by the brain-bone-blood triad via stress signals controls the bone marrow reservoir of immature and maturing leukocytes.
Mobilized peripheral blood is enriched with hematopoietic stem and progenitor cells which are essential for reconstitution in patients, and serves as a primary source for bone marrow transplantation procedures. The process, by which hematopoietic stem cells and progenitors egress out of the bone marrow to the circulation, and its enhancement by mobilization protocols, is not trivial and is regarded today as a highly regulated process involving multiple players, such as osteoblastosteoclast interactions, the chemokine SDF-1 and its major receptor CXCR4, and a complex cross-talk between cytokines, proteolytic enzymes and adhesion molecules. In this chapter, we will review clinical stem cell mobilization in brief, discuss experimental animal models, such as immune-deficient mice transplanted with human progenitor cells, as well as promising novel mobilizing agents, such as the CXCR4 antagonist AMD3100. In addition, we will focus on the molecular mechanistic aspect of stem cell mobilization, involving dynamic regulation of hematopoietic stem cells and the bone marrow microenvironment by the nervous and immune systems. A better understanding of these mechanisms will enable improvement of clinical mobilization protocols in the future.
2009
The nervous system regulates immunity through hormonal and neuronal routes as part of host defense and repair mechanism. Here, we review the emerging evidence for regulation of human hematopoietic stem and progenitor cells (HSPC) by the nervous system both directly and indirectly via their bone marrow (BM) niche-supporting stromal cells. Functional expression of several neurotransmitter receptors was demonstrated on HSPC, mainly on the more primitive CD34+/CD38-/low fraction. The myeloid cytokines, G-CSF and GM-CSF, dynamically upregulate neuronal receptor expression on human HSPC. This is followed by an increased response to neurotransmitters, leading to enhanced proliferation and motility of human CD34+ progenitors, repopulation of the murine BM and their egress to the circulation. Importantly, recent observations showed rapid mobilization of human HSPC to high SDF-1 expressing ischemic tissues of stroke individuals followed by neoangiogenesis, neurological and functional recovery. Along with decreased levels of circulating immature CD34+ cells and SDF-1 blood levels found in patients with early-stage Alzheimer's disease, these findings suggest a possible involvement of human HSPC in brain homeostasis and thus their potential clinical applications in neuropathology.
The mechanisms governing hematopoietic progenitor cell mobilization are not fully understood. We report higher membrane type 1-MMP (MT1-MMP) and lower expression of the MT1-MMP inhibitor, reversioninducing cysteine-rich protein with Kazal motifs (RECK), on isolated circulating human CD34+ progenitor cells compared with immature BM cells. The expression of MT1-MMP correlated with clinical mobilization of CD34+ cells in healthy donors and patients with lymphoid malignancies. Treatment with G-CSF further increased MT1-MMP and decreased RECK expression in human and murine hematopoietic cells in a PI3K/ Akt-dependent manner, resulting in elevated MT1-MMP activity. Blocking MT1-MMP function by Abs or siRNAs impaired chemotaxis and homing of G-CSF-mobilized human CD34+ progenitors. The mobilization of immature and maturing human progenitors in chimeric NOD/SCID mice by G-CSF was inhibited by anti-MT1-MMP treatment, while RECK neutralization promoted motility and egress of BM CD34+ cells. BM c-kit+ cells from MT1-MMP-deficient mice also exhibited inferior chemotaxis, reduced homing and engraftment capacities, and impaired G-CSF-induced mobilization in murine chimeras. Membranal CD44 cleavage by MT1-MMP was enhanced following G-CSF treatment, reducing CD34+ cell adhesion. Accordingly, CD44-deficient mice had a higher frequency of circulating progenitors. Our results reveal that the motility, adhesion, homing, and mobilization of human hematopoietic progenitor cells are regulated in a cell-autonomous manner by dynamic and opposite changes in MT1-MMP and RECK expression.
2008
Physiological interactions between the nervous and immune systems with components of the local microenvironment are needed to maintain homeostasis throughout the body. Dynamic regulation of bone remodeling, hematopoietic stem cells, and their evolving niches via neurotransmitter signaling are part of the host defense and repair mechanisms. This crosstalk links activated leukocytes, neuronal, and stromal cells, which combine to directly and indirectly regulate hematopoietic stem cells. Together, interactions between diverse systems create a regulatory "brain-bone-blood triad," contributing an additional dimension to the concept of the hematopoietic stem cell niche.
Therapeutic mobilization of vasculogenic progenitor cells is a novel strategy to enhance neovascularization for tissue repair. Prototypical mobilizing agents such as granulocyte colony-stimulating factor mobilize vasculogenic progenitor cells from the bone marrow concomitantly with inflammatory cells. In the bone marrow, mobilization is regulated in the stem cell niche, in which endosteal cells such as osteoblasts and osteoclasts play a key role. Because Wnt signaling regulates endosteal cells, we examined whether the Wnt signaling antagonist Dickkopf (Dkk)-1 is involved in the mobilization of vasculogenic progenitor cells. Using TOP-GAL transgenic mice to determine activation of β-catenin, we demonstrate that Dkk-1 regulates endosteal cells in the bone marrow stem cell niche and subsequently mobilizes vasculogenic and hematopoietic progenitors cells without concomitant mobilization of inflammatory neutrophils. The mobilization of vasculogenic progenitors required the presence of functionally active osteoclasts, as demonstrated in PTPϵ-deficient mice with defective osteoclast function. Mechanistically, Dkk-1 induced the osteoclast differentiation factor RANKL, which subsequently stimulated the release of the major bone-resorbing protease cathepsin K. Eventually, the Dkk-1-induced mobilization of bone marrow-derived vasculogenic progenitors enhanced neovascularization in Matrigel plugs. Thus, these data show that Dkk-1 is a mobilizer of vasculogenic progenitors but not of inflammatory cells, which could be of great clinical importance to enhance regenerative cell therapy.
The CD45 phosphatase is uniquely expressed by all leukocytes, but its role in regulating hematopoietic progenitors is poorly understood. We show that enhanced CD45 expression on bone marrow (BM) leukocytes correlates with increased cell motility in response to stress signals. Moreover, immature CD45 knockout (KO) cells showed defective motility, including reduced homing (both steady state and in response to stromal-derived factor 1) and reduced granulocyte colony-stimulating factor mobilization. These defects were associated with increased cell adhesion mediated by reduced matrix metalloproteinase 9 secretion and imbalanced Src kinase activity. Poor mobilization of CD45KO progenitors by the receptor activator of nuclear factor κB ligand, and impaired modulation of the endosteal components osteopontin and stem cell factor, suggested defective osteoclast function. Indeed, CD45KO osteoclasts exhibited impaired bone remodeling and abnormal morphology, which we attributed to defective cell fusion and Src function. This led to irregular distribution of metaphyseal bone trabecules, a region enriched with stem cell niches. Consequently, CD45KO mice had less primitive cells in the BM and increased numbers of these cells in the spleen, yet with reduced homing and repopulation potential. Uncoupling environmental and intrinsic defects in chimeric mice, we demonstrated that CD45 regulates progenitor movement and retention by influencing both the hematopoietic and nonhematopoietic compartments.
Aminoglycoside-arginine conjugates (AACs) are multi-target HIV-1 inhibitors. The most potent AAC is neomycin hexa-arginine conjugate, NeoR6. We here demonstrate that NeoR6 interacts with CXCR4 without affecting CXCL12-CXCR4 ordinary chemotaxis activity or loss of CXCR4 cell surface expression. Importantly, NeoR6 alone does not affect cell migration, indicating that NeoR6 interacts with CXCR4 at a distinct site that is important for HIV-1 entry and mAb 12G5 binding, but not to CXCL12 binding or signaling sites. This is further supported by our modeling studies, showing that NeoR6 and CXCL12 bind to two distinct sites on CXCR4, in contrast with other CXCR4 inhibitors, e.g. T140 and AMD3100. This complementary utilization of chemical, biology, and computation analysis provides a powerful approach for designing anti-HIV-1 drugs without interfering with the natural function of CXCL12/CXCR4 binding.
Heparanase is involved in tumor growth and metastasis. Because of its unique cleavage of heparan sulfate, which binds cytokines, chemokines and proteases, we hypothesized that heparanase is also involved in regulation of early stages of hematopoiesis. We report reduced numbers of maturing leukocytes but elevated levels of undifferentiated Sca-1+/c-Kit+/ Lin- cells in the bone marrow (BM) of mice overexpressing heparanase (hpa-Tg). This resulted from increased proliferation and retention of the primitive cells in the BM microenvironment, manifested in increased SDF-1 turnover. Furthermore, heparanase overexpression in mice was accompanied by reduced protease activity of MMP-9, elastase, and cathep- sin K, which regulate stem and progenitor cell mobilization. Moreover, increased retention of the progenitor cells also resulted from up-regulated levels of stem cell factor (SCF) in the BM, in particular in the stem cell-rich endosteum and endothelial regions. Increased SCF-induced adhesion of primitive Sca-1+/c- Kit+/Lin- cells to osteoblasts was also the result of elevation of the receptor c-Kit. Regulation of these phenomena is mediated by hyper- phosphorylation of c-Myc in hematopoietic progenitors of hpa-Tg mice or after exogenous heparanase addition to wild- type BM cells in vitro. Altogether, our data suggest that heparanase modification of the BM microenvironment regulates the retention and proliferation of hematopoietic progenitor cells.
2007
Only a subset of hierarchically arranged, primitive human AML progenitor cells can initiate the disease in transplanted immune-deficient mice. A publication in Nature Biotechnology by Ishikawa et al. (2007) describes a new animal model to study chemotherapy-resistant, quiescent human AML CD34+CD38- stem cells, which are retained in the endosteum region.
Catecholamines are important regulators of homeostasis, yet their functions in hematopoiesis are poorly understood. Here we report that immature human CD34+ cells dynamically expressed dopamine and β2-adrenergic receptors, with higher expression in the primitive CD34+CD38lo population. The myeloid cytokines G-CSF and GM-CSF upregulated neuronal receptor expression on immature CD34+ cells. Treatment with neurotransmitters increased the motility, proliferation and colony formation of human progenitor cells, correlating with increased polarity, expression of the metalloproteinase MT1-MMP and activity of the metalloproteinase MMP-2. Treatment with catecholamines enhanced human CD34+ cell engraftment of NOD-SCID mice through Wnt signaling activation and increased cell mobilization and bone marrow Sca-1+ c-Kit+Lin- cell numbers. Our results identify new functions for neurotransmitters and myeloid cytokines in the direct regulation of human and mouse progenitor cell migration and development.
Bone remodeling by bone-forming osteoblasts and bone-resorbing osteoclasts dynamically alters the bone inner wall and the endosteum region, which harbors osteoblastic niches for hematopoietic stem cells. Investigators have recently elucidated mechanisms of recruitment and mobilization; these mechanisms consist of stress signals that drive migration of leukocytes and progenitor cells from the bone marrow reservoir to the circulation and drive their homing to injured tissues as part of host defense and repair. The physical bone marrow vasculature barrier that is crossed by mobilized cells actively transmits chemotactic signals between the blood and the bone marrow, facilitating organ communication and cell trafficking. Osteoclasts play a dual role in regulation of bone resorption and homeostatic release or stress-induced mobilization of hematopoietic stem/progenitor cells. In this review, we discuss the orchestrated interplay between bone remodeling, the immune system, and the endosteal stem cell niches in the context of stem cell proliferation and migration during homeostasis, which are accelerated during alarm situations.
2006
Stromal cell-derived factor-1 (SDF-1/CXCL12) and its receptor CXCR4 are implicated in the pathogenesis and prognosis of acute myelogenous leukemia (AML). Cellular microparticles, submicron vesicles shed from the plasma membrane of various cells, are also associated with human pathology. In the present study, we investigated the putative relationships between the SDF-1/CXCR4 axis and microparticles in AML. We detected CXCR4-expressing microparticles (CXCR4+ microparticles) in the peripheral blood and bone marrow plasma samples of normal donors and newly diagnosed adult AML patients. In samples from AML patients, levels of CXCR4+ microparticles and total SDF-1 were elevated compared with normal individuals. The majority of CXCR4 + microparticles in AML patients were CD45+, whereas in normal individuals, they were mostly CD41+. Importantly, we found a strong correlation between the levels of CXCR4+ microparticle and WBC count in the peripheral blood and bone marrow plasma obtained from the AML patients. Of interest, levels of functional, noncleaved SDF-1 were reduced in these patients compared with normal individuals and also strongly correlated with the WBC count. Furthermore, our data indicate NH2-terminal truncation of the CXCR4 molecule in the microparticles of AML patients. However, such microparticles were capable of transferring the CXCR4 molecule to AML-derived HL-60 cells, enhancing their migration to SDF-1 in vitro and increasing their homing to the bone marrow of irradiated NOD/SCID/β2m null mice. The CXCR4 antagonist AMD3100 reduced these effects. Our findings suggest that functional CXCR4+ microparticles and SDF-1 are involved in the progression of AML. We propose that their levels are potentially valuable as an additional diagnostic AML variable.
The p53 tumor suppressor acts as a major barrier against cancer. To a large extent, this is due to its ability to maintain genome stability and to eliminate cancer cells from the replicative pool through cell-autonomous mechanisms. However, in addition to its well-documented functions within the malignant cancer cell, p53 can also exert non-cell-autonomous effects that contribute to tumor suppression. We now report that p53 can suppress the production of the chemokine SDF-1 in cultured fibroblasts of both human and mouse origin. This is due to a p53-mediated down-regulation of SDF-1 mRNA, which can be exacerbated on activation of p53 by the drug Nutlin-3. SDF-1 promotes the migration and invasiveness of cells that express its cognate receptor CXCR4. Indeed, medium conditioned by p53-deficient fibroblasts induces cancer cells towards increased directional migration and invasiveness, which are largely reversed by CXCR4 antagonist peptides. Because SDF-1 produced by stromal fibroblasts plays an important role in cancer progression and metastasis, our findings suggest that the ability of p53 to suppress stromal SDF-1 production may be an important mechanism whereby it does its non-cell-autonomous tumor suppressor function.
The chemokine SDF-1 (CXCL12) and its receptor CXCR4 are involved in regulation of migration, survival, and development of multiple cell types, including human hematopoietic CD34+/CD38-/low and stromal STRO-1+ stem cells. During steady-state homeostasis, CXCR4 is expressed by hematopoietic cells and also by stromal cells, which are the main source for SDF-1 in the bone marrow (BM). Stress-induced modulations in SDF-1 and CXCR4 levels participate in recruitment of immature and maturing leukocytes from the BM reservoir to damaged organs as part of host defense and repair mechanism. In addition, trafficking of SDF-1 is mediated by CXCR4, expressed by endothelial and various stromal cell types in the BM, spleen, and other organs, but not by hematopoietic cells. Transcytosis of functional SDF-1 to the BM takes place also in the stem cell-rich endothelium and endosteum regions, regulating hematopoietic and stromal interactions in the stem cell niche. Dynamic levels of SDF-1 and CXCR4 expression induce proliferation of hematopoietic and mesenchymal progenitors, recruitment of bone-resorbing osteoclasts, osteoblasts, neutrophils, and other myeloid cells, leading to leukocyte mobilization. These studies will be reviewed together with the mechanisms that regulate SDF-1 and CXCR4 physiologic function, inactivation, presentation, and availability. Moreover, the role and the dynamic modulations of this ligand and its receptor in alarm and pathologic conditions will be discussed as well.
Here we investigated the potential role of bone-resorbing osteoclasts in homeostasis and stress-induced mobilization of hematopoietic progenitors. Different stress situations induced activity of osteoclasts (OCLs) along the stem cell-rich endosteum region of bone, secretion of proteolytic enzymes and mobilization of progenitors. Specific stimulation of OCLs with RANKL recruited mainly immature progenitors to the circulation in a CXCR4- and MMP-9-dependent manner; however, RANKL did not induce mobilization in young female PTPε-knockout mice with defective OCL bone adhesion and resorption. Inhibition of OCLs with calcitonin reduced progenitor egress in homeostasis, G-CSF mobilization and stress situations. RANKL-stimulated bone-resorbing OCLs also reduced the stem cell niche components SDF-1, stem cell factor (SCF) and osteopontin along the endosteum, which was associated with progenitor mobilization. Finally, the major bone-resorbing proteinase, cathepsin K, also cleaved SDF-1 and SCF. Our findings indicate involvement of OCLs in selective progenitor recruitment as part of homeostasis and host defense, linking bone remodeling with regulation of hematopoiesis.
To study the role of the stress-induced "readthrough" acetylcholinesterase splice variant, AChE-R, in thrombopoiesis, we used transgenic mice overexpressing human AChE-R (TgR). Increased AChE hydrolytic activity in the peripheral blood of TgR mice was associated with increased thrombopoietin levels and platelet counts. Bone marrow (BM) progenitor cells from TgR mice presented an elevated capacity to produce mixed (GEMM) and megakaryocyte (Mk) colonies, which showed intensified labeling of AChE-R and its interacting proteins RACK1 and PKC. When injected with bacterial lipopolysaccharide (LPS), parent strain FVB/N mice, but not TgR mice, showed reduced platelet counts. Therefore, we primed human CD34+ cells with the synthetic ARP26 peptide, derived from the cleavable C-terminus of AChE-R prior to transplantation, into sublethally irradiated NOD/SCID mice. Engraftment of human cells (both CD45+ and CD41+ Mk) was significantly increased in mice that received ARP26-primed CD34 + human cells versus mice that received fresh nonprimed CD34 + human cells. Moreover, ARP26 induced polyploidization and proplatelet shedding in human MEG-01 promegakaryotic cells, and human platelet engraftment increased following ex vivo expansion of ARP 26-treated CD34+ cells as compared to cells expanded with thrombopoietin and stem cell factor. Our findings implicate AChE-R in thrombopoietic recovery, suggesting new therapeutic modalities for supporting platelet production.
Chemokines are key regulators of hematopoiesis and host defense. We report here that functional expression of the chemokine receptor CXCR4 on human immature CD34+ hematopoietic progenitors was increased as a result of sustained elevation in cellular cAMP by db-cAMP and prostaglandin E2. This effect of cAMP was specifically mediated by PKCδ activity. CXCR4 expression and PKCδ activation by cAMP were decreased after the inhibition of cAMP effector-Rap1 by Spa1 overexpression. Interference with the activation of Rac1, a downstream target of Rap1, prevented the cAMP-induced increase in PKCδ activity and CXCR4 levels. Functional manifestation of the effects of cAMP-elevating agents revealed an increased ability of human CD34+ cells to transmigrate the bone marrow (BM) endothelial layer and adhere to BM stroma in vitro, and it augmented the homing potential to the BM and spleens of immunodeficient mice in a Rac1- and a PKCδ-dependent manner. cAMP- and TNFα-stimulated pathways converged in PKCδ-activated CXCR4 expression and MMP-2/MMP-9 secretion. cAMP treatment had a beneficial effect on CD34+ cell survival in a PKCδ-mediated fashion. Taken together, our data reveal major roles for cAMP-induced PKCδ activation in signaling governing the motility and development of CD34+ cells.
Although hematopoietic progenitor/stem cells (HPC) have been used for autologous transplants for approximately 25 years, it is only recently that we have begun to finally understand the factors which play important roles in causing these cells to leave their marrow niches and circulate in the blood. Still less is understood about factors important in homing of these cells from the blood to the marrow, and their re-engraftment there. Nonetheless, a significant amount of clinical information exists on how to make these cells leave the marrow in order to facilitate their collection from the blood for use as a transplant graft. This review provides an overview of what is currently known about the factors influencing mobilization of HPC from the marrow into the blood. Further, it suggests how this knowledge may be used to individually optimize collection of HPC. It is particularly important to optimize collection in the older myeloma patient, where it has traditionally been difficult to collect adequate numbers of cells for the tandem transplant now thought to provide the best hope for long-term survival in this disease.
2005
Regulation of the availability of chemokine SDF-1 (CXCL12) in bone marrow is still not fully understood. Here we describe a unique function for the chemokine receptor CXCR4 expressed on bone marrow endothelial cells, which efficiently internalize circulating SDF-1, resulting in its translocation into the bone marrow. Translocated SDF-1 increased the homing of transplanted human CD34+ hematopoietic progenitors to the bone marrow. The chemokine transporter function of CXCR4 was a characteristic of endothelial and stromal cells but not of hematopoietic cells. Thus, chemokine translocation across the blood-bone marrow barrier allows effective transfer of functional SDF-1 from the periphery to the stem cell niche in the bone marrow during both homeostasis and 'alarm' situations.
Migration of hematopoietic stem cells through the blood, across the endothelial vasculature to different organs and to their bone marrow (BM) niches, requires active navigation, a process termed homing. Homing is a rapid process and is the first and essential step in clinical stem cell transplantation. Similarly, homing is required for seeding of the fetal BM by hematopoietic progenitors during development. Homing has physiological roles in adult BM homeostasis, which are amplified during stress-induced recruitment of leukocytes from the BM reservoir and during stem cell mobilization, as part of host defense and repair. Homing is thought to be a coordinated, multistep process, which involves signaling by stromal-derived factor 1 (SDF-1) and stem cell factor (SCF), activation of lymphocyte function-associated antigen 1 (LFA-1), very late antigen 4/5 (VLA-4/5) and CD44, cytoskeleton rearrangement, membrane type 1 (MT1)-matrix metalloproteinase (MMP) activation and secretion of MMP2/9. Rolling and firm adhesion of progenitors to endothelial cells in small marrow sinusoids under blood flow is followed by trans-endothelial migration across the physical endothelium/extracellular matrix (ECM) barrier. Stem cells finalize their homing uniquely, by selective access and anchorage to their specialized niches in the extravascular space of the endosteum region and in periarterial sites. This review is focused on mechanisms and key regulators of human stem cell homing to the BM in experimental animal models and clinical transplantation protocols.
The maintenance of bone marrow stromal stem cells (BMSSCs) is tightly controlled by the local microenvironment and by autocrine regulatory factors secreted by BMSSCs. To identify such factors, a cDNA subtraction library was generated from purified BMSSCs, based on their high expression of the STRO-1 antigen. Stromal-derived factor-1 (SDF-1) was one differentially expressed gene highly expressed by purified BMSSCs prior to culture. In vitro, immature preosteogenic cells expressed greater levels of SDF-1 when compared with mature cell types representative of osteoblasts and osteocytes/bone lining cells. Furthermore, SDF-1 expression was rapidly down-regulated when BMSSCs were cultured under osteoinductive conditions. BMSSCs were also shown to express functional cell surface SDF-1 receptors (CXCR4). Transduced BMSSC lines, secreting high SDF-1 levels, displayed an enhanced ability to form ectopic bone in vivo, in comparison with control BMSSC lines. Moreover, high SDF-1-expressing BMSSCs displayed an increased capacity for cellular growth and protection against interleukin-4-induced apoptosis. Similarly, fibroblast colony-forming units (CFU-Fs) also displayed increased growth and resistance to α-interferon-2a-induced apoptosis, in synergy with platelet-derived growth factor BB (PDGF-BB) and SDF-1 in vitro. These studies indicate that the chemokine, SDF-1, may play a role in the maintenance, survival, and osteogenic capacity of immature BMSSC populations.
Multiple myeloma (MM) is an incurable plasma cell (PC) malignancy able to mediate massive destruction of the axial and craniofacial skeleton. The aim of this study was to investigate the role of the potent chemokine, stromal-derived factor-1α (SDF-1α) in the recruitment of osteoclast precursors to the bone marrow. Our studies show that MM PC produce significant levels of SDF-1α protein and exhibit elevated plasma levels of SDF-1α when compared with normal, age-matched subjects. The level of SDF-1α positively correlated with the presence of multiple radiological bone lesions in individuals with MM, suggesting a potential role for SDF-1α in osteoclast precursor recruitment and activation. To examine this further, peripheral blood-derived CD14 + osteoclast precursors were cultured in an in vitro osteoclast-potentiating culture system in the presence of recombinant human SDF-1α. Although failing to stimulate an increase in TRAP +, multinucleated osteoclast formation, our studies show that SDF-1α mediated a dramatic increase in both the number and the size of the resorption lacunae formed. The increased osteoclast motility and activation in response to SDF-1α was associated with an increase in the expression of a number of osteoclast activation-related genes, including RANKL, RANK, TRAP, MMP-9, CA-II, and Cathepsin K. Importantly, the small-molecule CXCR4-specific inhibitor, 4F-Benzoyl-TE14011 (T140), effectively blocked osteoclast formation stimulated by the myeloma cell line, RPMI-8226. Based on these findings, we believe that the synthesis of high levels of SDF-1α by MM PC may serve to recruit osteoclast precursors to local sites within the bone marrow and enhance their motility and bone-resorbing activity. Therefore, we propose that inhibition of the CXCR4-SDF-1α axis may provide an effective means of treatment for MM-induced osteolysis.
The substantial understanding that has been gained over the past 5 decades of the biology of blood formation is largely due to the development of functional quantitative assays for cells at all stages of differentiation, from multipotential stem cells to mature cells. The majority of studies have involved the mouse because the ease with which repopulation studies can be carried out with this animal model allows the assay of complete lineage development from stem cells. In the past decade, advances in repopulation assays for human stem cells using xenotransplantation have greatly enhanced our understanding of human stem cell biology. Importantly, the xenotransplantation methodology has also been used to identify the cancer stem cell that initiates and sustains leukemic proliferation, providing key evidence for the cancer stem cell hypothesis. This hypothesis argues that cancer cells are functionally heterogeneous and hierarchically organized such that only specific cells are capable of sustaining tumor growth and continuously producing the cells that make up the bulk of the tumor. Recent studies have also brought into focus the importance of the intimate relationship between the stem cell (normal or leukemic) and its microenvironment. Coming into view are the molecular players involved in stem cell homing, migration, and adhesion, as well as the cellular components of the microenvironmental niche. Here we review recent studies that have begun to elucidate the interplay between normal and leukemic human stem cells and their microenvironment.
The chemokine stromal cell-derived factor-1 (SDF-1) and its receptor, CXCR4, play a major role in migration, retention, and development of hematopoietic progenitors in the bone marrow. We report the direct involvement of atypical PKC-ζ in SDF-1 signaling in immature human CD34 +-enriched cells and in leukemic pre-B acute lymphocytic leukemia (ALL) G2 cells. Chemotaxis, cell polarization, and adhesion of CD34+ cells to bone marrow stromal cells were found to be PKC-ζ dependent. Overexpression of PKC-ζ in G2 and U937 cells led to increased directional motility to SDF-1. Interestingly, impaired SDF-1-induced migration of the pre-B ALL cell line B1 correlated with reduced PKC-ζ expression. SDF-1 triggered PKC-ζ phosphorylation, translocation to the plasma membrane, and kinase activity. Furthermore we identified PI3K as an activator of PKC-ζ, and Pyk-2 and ERK1/2 as downstream targets of PKC-ζ. SDF-1-induced proliferation and MMP-9 secretion also required PKC-ζ activation. Finally, we showed that in vivo engraftment, but not homing, of human CD34 +-enriched cells to the bone marrow of NOD/SCID mice was PKC-ζ dependent and that injection of mice with inhibitory PKC-ζ pseudosubstrate peptides resulted in mobilization of murine progenitors. Our results demonstrate a central role for PKC-ζ in SDF-1-dependent regulation of hematopoietic stem and progenitor cell motility and development.
2004
Trafficking of human CD34+ stem/progenitor cells (HSCS/HPCs) is regulated by chemokines, cytokines, proteolytic enzymes, and adhesion molecules. We report that the adhesion receptor CD44 and its major ligand, hyaluronlc acid (HA), are essential for homing into the bone marrow (BM) and spleen of nonobese diabetic/severe combined immunodeficient (NOD/SCID) mice and engraftment by human HSCs. Homing was blocked by anti-CD44 monoclonal antibodies (mAbs) or by soluble HA, and it was significantly impaired after intravenous injection of hyaluronidase. Furthermore, stromal cell-derived factor-1 (SDF-1) was found to be a rapid and potent stimulator of progenitor adhesion to immobilized HA, leading to formation of actin-containing protrusions with CD44 located at their tips. HPCs migrating on HA toward a gradient of SDF-1 acquired spread and polarized morphology with CD44 concentrating at the pseudopodia at the leading edge. These morphologic alterations were not observed when the progenitors were first exposed to anti-CD44 mAbs, demonstrating a crosstalk between CD44 and CXCR4 signaling. Unexpectedly, we found that HA is expressed on human BM sinusoidal endothelium and endosteum, the regions where SDF-1 is also abundant. Taken together, our data suggest a key role for CD44 and HA in SDF-1-dependent transendothelial migration of HSCs/HPCs and their final anchorage within specific niches of the BM.
The mechanisms governing migration and extramedullary dissemination of leukemic cells remain obscure. In this study the migration and in vivo homing to the bone marrow of nonobese diabetic severe combined immunodeficient (NOD/SCID) mice injected with human precursor-B acute lymphoblastic leukemia (ALL) cells in comparison to normal CD34+ progenitors (both cord blood and mobilized peripheral blood) was investigated. Although migration and homing of both cell populations was dependent on stromal cell-derived factor 1 (SDF-1)/CXCR4 interactions, major differences in receptor expression as well as the migratory capacity toward various concentrations of SDF-1 were found. Furthermore, unlike normal CD34+ progenitors, in vivo homing of the leukemic cells was superior when recipient NOD/SCID mice were not irradiated prior to transplantation. In addition, we report differences in the adhesion molecules activated following SDF-1 stimulation, documenting a major role for very late antigen 4 (VLA-4), but not VLA-5 and lymphocyte function-associated antigen-1 (LFA-1), in homing of precursor-B ALL cells. Interestingly, Toxin-B and pertussis toxin inhibited the homing of the leukemic cells but not that of normal CD34+ progenitors or normal CD10+/CD19+ precursor-B cells, revealing differences in CXCR4 signaling pathways that are based on changes that acquired by the leukemic cells. Altogether, our data provide new insights into different SDF-1-induced signaling, activation, and consequent motility between normal CD34+ and precursor-B ALL progenitors, which may lead to improved clinical protocols.
The chemokine stromal cell-derived factor-1 (SDF-1) and its receptor CXCR4 participate in the retention of normal hematopoietic stem cells within the bone marrow (BM) and their release into the circulation. Homing and engraftment of human stem cells in immunodeficient mice are dependent on cell surface CXCR4 expression and the production of BM SDF-1, which acts also as a survival factor for both human and murine stem cells. However, the role of SDF-1/CXCR4 interactions in the control of human acute myelogenous leukemia (AML) cell trafficking and disease progression is poorly understood. In this study, we report that although some AML cells do not express surface CXCR4, all AML cells tested express internal CXCR4 and SDF-1. Culture of AML cells with SDF-1 promoted their survival, whereas addition of neutralizing CXCR4 antibodies, SDF-1 antibodies, or AMD3100 significantly decreased it. Pretreatment of primary human AML cells with neutralizing CXCR4 antibodies blocked their homing into the BM and spleen of transplanted NOD/SCID/B2m null mice. Furthermore, weekly administrations of anti-human CXCR4 to mice previously engrafted with primary AML cells led to a dramatic decrease in the levels of human AML cells in the BM, blood, and spleen in a dose- and time-dependent manner. Interestingly, the same treatment did not affect significantly the levels of normal human progenitors engrafted into NOD/SCID mice. Taken together, our findings demonstrated the importance of the SDF-1/CXCR4 axis in the regulation of in vivo motility and development of human AML stem cells and identified CXCR4 neutralization as a potential treatment for AML.
A major limitation to clinical stem cell-mediated gene therapy protocols is the low levels of engraftment by transduced progenitors. We report that CXCR4 overexpression on human CD34+ progenitors using a lentiviral gene transfer technique helped navigate these cells to the murine bone marrow and spleen in response to stromal-derived factor 1 (SDF-1) signaling. Cells overexpressing CXCR4 exhibited significant increases in SDF-1-mediated chemotaxis and actin polymerization compared with control cells. A major advantage of CXCR4 overexpression was demonstrated by the ability of transduced CD34+ cells to respond to lower, physiologic levels of SDF-1 when compared to control cells, leading to improved SDF-1-induced migration and proliferation/survival, and finally resulting in significantly higher levels of in vivo repopulation of nonobese diabetic/severe combined immunodeficiency (NOD/SCID) mice including primitive CD34+/CD38-/low cells. Importantly, no cellular transformation was observed following transduction with the CXCR4 vector. Unexpectedly, we documented lack of receptor internalization in response to high levels of SDF-1, which can also contribute to increased migration and proliferation by the transduced CD34+ cells. Our results suggest CXCR4 overexpression for improved definitive human stem cell motility, retention, and multilineage repopulation, which could be beneficial for in vivo navigation and expansion of hematopoietic progenitors.
2003
Hematopoietic stem cells rarely contribute to hepatic regeneration, however, the mechanisms governing their homing to the liver, which is a crucial first step, are poorly understood. The chemokine stromal cell-derived factor-1 (SDF-1), which attracts human and murine progenitors, is expressed by liver bile duct epithelium. Neutralization of the SDF-1 receptor CXCR4 abolished homing and engraftment of the murine liver by human CD34+ hematopoietic progenitors, while local injection of human SDF-1 increased their homing. Engrafted human cells were localized in clusters surrounding the bile ducts, in close proximity to SDF-1-expressing epithelial cells, and differentiated into albumin-producing cells. Irradiation or inflammation increased SDF-1 levels and hepatic injury induced MMP-9 activity, leading to both increased CXCR4 expression and SDF-1-mediated recruitment of hematopoietic progenitors to the liver. Unexpectedly, HGF, which is increased following liver injury, promoted protrusion formation, CXCR4 upregulation, and SDF-1-mediated directional migration by human CD34+ progenitors, and synergized with stem cell factor. Thus, stress-induced signals, such as increased expression of SDF-1, MMP-9, and HGF, recruit human CD34+ progenitors with hematopoietic and/or hepatic-like potential to the liver of NOD/SCID mice. Our results suggest the potential of hematopoietic CD34+/CXCR4 + cells to respond to stress signals from non-hematopoietic injured organs as an important mechanism for tissue targeting and repair.
One of the major problems limiting stem cellbased therapies, beyond simple transplantation of mononuclear cells or positive selection of CD34 cells, is the absence of a clear understanding of the composition of the stem cell (HSC) pool in humans. The right cell must be targeted for the right therapy. For gene therapy, HSCs capable of permanent repopulation must be transduced, whereas for cancer therapy an HSC capable of rapidly generating granulocytes, platelets, and erythroid cells is also required....
Successful blood and marrow transplant (BMT), both autologous and allogeneic, requires the infusion of a sufficient number of hematopoietic progenitor/stem cells (HPCs) capable of homing to the marrow cavity and regenerating a full array of hematopoietic cell lineages in a timely fashion. At present, the most commonly used surrogate marker for HPCs is the cell surface marker CD34, identified in the clinical laboratory by flow cytometry. Clinical studies have shown that infusion of at least 2 x 10(6) CD34(+) cells/kg recipient body weight results in reliable engraftment as measured by recovery of adequate neutrophil and platelet counts approximately 14 days after transplant. Recruitment of HPCs from the marrow into the blood is termed mobilization, or, more commonly, stem cell mobilization. In Section I, Dr. Tsvee Lapidot and colleagues review the wide range of factors influencing stem cell mobilization. Our current understanding focuses on chemokines, proteolytic enzymes, adhesion molecules, cytokines and stromal cell-stem cell interactions. On the basis of this understanding, new approaches to mobilization have been designed and are now starting to undergo clinical testing. In Section II, Dr. Michele Cottler-Fox describes factors predicting the ability to mobilize the older patient with myeloma. In addition, clinical approaches to improving collection by individualizing the timing of apheresis and adjusting the volume of blood processed to achieve a desired product are discussed. Key to this process is the daily enumeration of blood CD34(+) cells. Newer methods of enumerating and mobilizing autologous blood HPCs are discussed. In Section III, Dr. John DiPersio and colleagues provide data on clinical results of mobilizing allogeneic donors with G-CSF, GM-CSF and the combination of both as relates to the number and type of cells collected by apheresis. Newer methods of stem cell mobilization as well as the relationship of graft composition on immune reconstitution and GVHD are discussed.
2002
Homing and repopulation of nonobese diabetic/severe combined immunodeficient (NOD/SCID) mice by enriched human CD34+ stem cells from cord blood, bone marrow, or mobilized peripheral blood are dependent on stromal cellderived factor 1 (SDF-1)/CXCR4 interactions. Recently, human cord and fetal blood CD34+CD38-CXCR4- and CXCR4+ cells, sorted with neutralizing anti-CXCR4 monoclonal antibody (mAb), were shown to have similar NOD/SCID repopulation potential. Herein we report that human cord blood CD34+CXCR4+ (R4+) and CD34+CXCR4- (R4-) subsets, sorted with neutralizing anti-CXCR4 mAb, engrafted NOD/SCID mice with significantly lower levels of human cells compared with nonsorted and SDF-1-migrated CD34+ cells. Coinjection of purified cells with 10 μg anti-CXCR4 mAb significantly reduced engraftment of all CD34+ subsets, and 50 μg completely abrogated engraftment by R4- and CD34+ cells. Importantly, R4- cells harbor intracellular CXCR4, which can be rapidly induced to cell surface expression within a few hours. Moreover, 48 hours of cytokine stimulation resulted in up-regulation of both cell surface and intracellular CXCR4, restoring migration capacities toward a gradient of SDF-1 and high-level NOD/SCID repopulation potential. In addition, homing of sorted R4- cells into the murine bone marrow and spleen was significantly slower and reduced compared to CD34+ cells but yet CXCR4 dependent. In conclusion, R4- cells express intracellular CXCR4, which can be functionally expressed on the cell membrane to mediate SDF-1-dependent homing and repopulation. Our results suggest dynamic CXCR4 expression on CD34+ stem and progenitor cells, regulating their motility and repopulation capacities.
Hematopoietic stem cells are identified based on their functional ability to migrate via the blood circulation of transplanted recipients, to home to the host bone marrow and to durably repopulate this organ with high levels of maturing myeloid and lymphoid cells. While a small pool of undifferentiated stem cells with the potential to repeat the entire process in serially transplanted recipients is maintained within the bone marrow, maturing cells are continuously released into the circulation. In recent years pre-clinical, functional in vivo models for human stem cells have been developed, using immune-deficient mice or pre-immune, fetal sheep as recipients. The mechanism of human stem cell migration, homing and repopulation in transplanted immune-deficient NOD/SCID and NOD/SCID/B2mnull mice as well as the accessory mediators that facilitate these processes, will be reviewed. In particular, the essential roles of the chemokine SDF-1 and its receptor CXCR4 which mediate and regulate stem cell homing and repopulation will be discussed.
Mobilization of hematopoietic stem and progenitor cells from the bone marrow into the circulation by repetitive, daily stimulations with G-CSF alone, or in combination with cyclophosphamide, is increasingly used clinically; however, the mechanism is not fully understood. Moreover, following mobilization stem cells also home back to the bone marrow, suggesting that stem cell release/mobilization and homing are sequential events with physiological roles. Previously, a role for cytokines such as G-CSF and SCF, and adhesion molecules such as VLA-4 and P/E selectins, was determined for stem cell mobilization. Recent results using experimental animal models and samples from clinical mobilization protocols demonstrate major involvement of chemokines such as stromal derived factor-1 (SDF-1) and IL-8, as well as proteolytic enzymes such as elastase, cathepsin G, and various MMPs in the mobilization process. These results will be reviewed together with the central roles of SDF-1 and CXCR4 interactions in G-CSF or G-CSF in combination with cyclophosphamide-induced mobilization. Furthermore, the central role of this chemokine in stem cell homing to the bone marrow as well as retention of undifferentiated cells within this tissue will also be discussed.
2001
Stem cell homing into the bone microenvironment is the first step in the initiation of marrow-derived blood cells. It is reported that human severe combined immunodeficient (SCID) repopulating cells home and accumulate rapidly, within a few hours, in the bone marrow and spleen of immunodeficient mice previously conditioned with total body irradiation. Primitive CD34+CD38-/lowCXCR4+ cells capable of engrafting primary and secondary recipient mice selectively homed to the bone marrow and spleen, whereas CD34-CD38-/lowLin- cells were not detected. Moreover, whereas freshly isolated CD34+CD38+/high cells did not home, in vivo stimulation with granulocyte colony-stimulating factor as part of the mobilization process, or in vitro stem cell factor stimulation for 2 to 4 days, potentiated the homing capabilities of cytokine-stimulated CD34+CD38+ cells. Homing of enriched human CD34+ cells was inhibited by pretreatment with anti-CXCR4 antibodies. Moreover, primitive CD34+-CD38-/lowCXCR4+ cells also homed in response to a gradient of human stromal cell-derived factor 1 (SDF-1), directly injected into the bone marrow or spleen of nonirradiated NOD/SCID mice. Homing was also inhibited by pretreatment of CD34+ cells with antibodies for the major integrins VLA-4, VLA-5, and LFA-1. Pertussis toxin, an inhibitor of signals mediated by Gαi proteins, inhibited SDF-1-mediated in vitro transwell migration but not adhesion or in vivo homing of CD34+ cells. Homing of human CD34+ cells was also blocked by chelerythrine chloride, a broad-range protein kinase C inhibitor. This study reveals rapid and efficient homing to the murine bone marrow by primitive human CD34+CD38-/lowCXCR4+ cells that is integrin mediated and depends on activation of the protein kinase C signal transduction pathway by SDF-1.
Five specific single-chain antibodies recognizing the human vascular endothelial growth factor receptor-2 (VEGFR-2/KDR) were selected from a V-gene phage display library constructed from mice immunized with file extracellular domain of VEGFR-2 (Ig-like domain 1-7). All five scFv antibodies (A2, A7, B11, G3, and H1) bound to the purified native antigen in enzyme-linked immunosorbent assay and Dot Blot, and showed no crossreactivity to the human VEGF-receptor 1 (VEGFR-1). The selected antibodies recognize a conformation-dependent epitope of the native receptor and do not recognize denatured antigen in Western blots, as well as linear overlapping peptides comprising the sequence of the human VEGFR-2. The five scFv antibodies bind to the surface of endothelial cells overexpressing human VEGFR-2 c-DNA (PAE/VEGFR-2 cells) as detected by surface immunofluorescence using confocal microscopy. In addition scFv A7 specifically detected VEGFR-2 expressing endothelial cells in the glomerulus of frozen human kidney tissue sections. Therefore, A7 has potential clinical application as a marker for angiogenesis in cryosections of different human tissues. Additionally, two recombinant scFvs (A2 and A7) very efficiently recognize VEGFR-2 on PAE/VEGFR-2 cells and freshly prepared human umbilical vein endothelial cells by fluorescence-activated cell sorter (FACS) analysis. The scFv fragment A7, which was the most sensitive antibody in FACS analysis, recognizes human CD34+VEGFR-2+ hematopoietic immature cells within the population of enriched CD34+ cells isolated from human cord blood. The dissociation constant of A7 was determined to be Kd = 3.8 × 10-9 M by BIAcore analysis. In conclusion, scFv fragment A7 seems to be an important tool for FACS analysis and cell sorting of vascular endothelial cells, progenitor cells and hematopoitic stem cells, which are positive for VEGFR-2 gene expression.
The mechanism of hematopoietic stem cell migration and repopulation is not fully understood. Murine fetuses that lack the chemokine stromal-derived factor one (SDF-1null) or its receptor CXCR4 (CXCR4null) have multiple defects that are lethal, including impaired bone marrow hematopoiesis. These results suggest a major role for SDF-1/CXCR4 interactions in murine stem cell homing from the fetal liver into the bone marrow and its repopulation during development. SDF-1 is highly conserved between different species. Human and murine SDF-1 are cross-reactive and differ in one amino acid. Recently, we reported that SDF-1 and CXCR4 are essential for homing and repopulation of immune-deficient NOD/SCID and B2mnull NOD/SCID mice by human stem cells. In addition, immature human CD34+ cells and primitive CD34+/CD38-/low cells, which do not migrate toward a gradient of SDF-1 in vitro, and do not home and repopulate in vivo the murine bone marrow, can become functional repopulating cells by short-term 16-48 hr in vitro stimulation with cytokines such as SCF and IL-6 prior to transplantation. These cytokines increase surface CXCR4 expression, migration toward SDF-1, and in vivo homing and repopulation. We discuss the pleiotropic roles of SDF-1/CXCR4 interactions in human stem cell migration, development, and repopulation in transplanted immune-deficient mice.
2000
Hematopoietic stem cell homing and engraftment require several adhesion interactions, which are not fully understood. Engraftment of nonobese/severe combined immunodeficiency (NOD/SCID) mice by human stem cells is dependent on the major integrins very late activation antigen-4 (VLA-4); VLA-5; and to a lesser degree, lymphocyte function associated antigen-1 (LFA-1). Treatment of human CD34+ cells with antibodies to either VLA-4 or VLA-5 prevented engraftment, and treatment with anti-LFA-1 antibodies significantly reduced the levels of engraftment. Activation of CD34+ cells, which bear the chemokine receptor CXCR4, with stromal derived factor 1 (SDF-1) led to firm adhesion and transendothelial migration, which was dependent on LFA-1/ICAM-1 (intracellular adhesion molecule-1) and VLA-4/VCAM-1 (vascular adhesion molecule-1). Furthermore, SDF-1-induced polarization and extravasation of CD34+/CXCR4+ cells through the extracellular matrix underlining the endothelium was dependent on both VLA-4 and VLA-5. Our results demonstrate that repopulating human stem cells functionally express LFA-1, VLA-4, and VLA-5. Furthermore, this study implies a novel approach to further advance clinical transplantation. (C) 2000 by The American Society of Hematology.
The chemokine stromal-derived factor-1 (SDF-1) controls many aspects of stem cell function. Details of its regulation and sites of production are currently unknown. We report that in the bone marrow, SDF-1 is produced mainly by immature osteoblasts and endothelial cells. Conditioning with DNAdamaging agents (ionizing irradiation, cyclophosphamide, and 5-fluorouracil) caused an increase in SDF-1 expression and in CXCR4-dependent homing and repopulation by human stem cells transplanted into NOD/SCID mice. Our findings suggest that immature osteoblasts and endothelial cells control stem cell homing, retention, and repopulation by secreting SDF-1, which also participates in host defense responses to DNA damage.
1999
Stem cell homing and repopulation are not well understood. The chemokine stromal cell-derived factor-1 (SDF-1) and its receptor CXCR4 were found to be critical for murine bone marrow engraftment by human severe combined immunodeficient (SCID) repopulating stem cells. Treatment of human cells with antibodies to CXCR4 prevented engraftment. In vitro CXCR4-dependent migration to SDF-1 of CD34+CD38-(/low) cells correlated with in vivo engraftment and stem cell function. Stem cell factor and interleukin-6 induced CXCR4 expression on CD34+ cells, which potentiated migration to SDF-1 and engraftment in primary and secondary transplanted mice. Thus, up-regulation of CXCR4 expression may be useful for improving engraftment of repopulating stem cells in clinical transplantation.
1998
We have previously shown that intravenously injected peripheral blood (PB) or bone marrow (BM) cells from newly diagnosed chronic myeloid leukemia (CML) patients can engraft the BM of sublethally irradiated severe combined immunodeficient (SCID) mice. We now report engraftment results for chronic phase CML cells in nonobese diabetic (NOD)/SCID recipients which show the superiority of this latter model. Transplantation of NOD/SCID mice with 7 to 10 x 107 patient PB or BM calls resulted in the continuing presence of human calls in the BM of the mice for up to 7 months, and primitive human CD34+ cells, including those detectable as colony-forming calls (CFC), as long- term culture-initiating cells, or by their coexpression of Thy-1, were found in a higher proportion of the NOD/SCID recipients analyzed, and at higher levels than were seen previously in SCID recipients. The human CFC and total human calls present in the BM of the NOD/SCID mice transplanted with CML cells also contained higher proportions of leukemic calls than were obtained in the SCID model, and NOD/SCID mice could be repopulated with transplants of enriched CD34+ cells from patients with CML. These results suggest that the NOD/SCID mouse may allow greater engraftment and amplification of both normal and leukemic (Ph+) calls sufficient for the quantitation and characterization of the normal and leukemic stem cells present in patients with CML. In addition, this model should make practical the investigation of mechanisms underlying progression of the disease and the development of more effective in vivo therapies.
The imrnune-rnediated effect of natural killer (NK) and cytotoxic T cells against residual tumor cells (GVL) has previously been shown to prevent relapse and reinduce remission post-BMT. Cord blood (CB) is a rich source of fetal NK cells (CD16"CD56+) with high lytic capabilities. CB transplantais (CBT) are reported to be associated with lower risk of graft versus host disease which may jeopardize the GVL effect. Therefore, our goal was to amplify CB-derived NK cell-mediated GVL,. CB-derived NK cells were separated using a-CD56 McAb and immunomagnetic beads. The cells were expanded in the presence of 1L-2 (1000 lU/ml). Maximal fold expansion (80.4±I6.6) was achieved on day 20±2 by culturing the cells in the presence of irradiated autologous lymphocytes while irradiated murine stromal cells yielded 54.7+8.4 fold expansion (p
1997
Based on initial observations of human CD34+ Thy-1+ cells and long- term culture-initiating cells (LTC-IC) in the bone marrow of some sublethally irradiated severe combined immunodeficient (SCID) mice transplanted intravenously with normal human marrow cells, and the subsequent finding that the NOD/LtSz-scid/scid (NOD/SCID) mouse supports higher levels of human cell engraftment, we undertook a series of time course experiments to examine posttransplant changes in the number, tissue distribution, cycling activity, and in vivo differentiation pattern of various human hematopoietic progenitor cell populations in this latter mouse model. These studies showed typical rapid posttransplant recovery curves for human CD34- CD19+ (B-lineage) cells, CD34+ granulopoietic, erythroid, and multilineage colony-forming cells (CFC), LTC-IC, and CD34+ Thy-1+ cells from a small initial population representing
The SJL/J mouse strain has a high spontaneous incidence of a B-cell neoplasm, reticulum cell neoplasm type B (RCN B). In addition, following irradiation, 10% to 30% of these mice develop acute myelomonocytic leukemia (radiation-induced acute myeloid leukemia [RI-AML]), an incidence that can be increased to 50% by treatment of the mice with corticosteroids after irradiation. The role played by the mononuclear phagocyte growth factor, colony-stimulating factor-1 (CSF-1), in the development of RI-AML in SJL/J mice was investigated. Mice dying of RI-AML, but not those dying of RCN B or without disease, possessed elevated concentrations of circulating CSF-1. In addition, in mice developing RI-AML with a more prolonged latency, circulating CSF-1 concentrations were increased before overt expression of RI-AML. First-passage tumors from 14 different RI-AMLs all contained high concentrations of CSF-1, and six of six different first- or second-passage tumors expressed the CSF-1 receptor (CSF-1R). Furthermore, in vitro colony formation by first- or second-passage tumor cells from 20 of 20 different RI- AMLs was blocked by neutralizing anti-CSF-1 antibody, and four of four of these tumors were inhibited by anti-CSF-1R antibody. The results of these antibody neutralization studies, coupled with the observation of elevated circulating CSF-1 in mice developing RI-AML, show an autocrine role for CSF- 1 in RI-AML development in SJL/J mice. Southern blot analysis of tumor DNA from six of six of these tumors failed to reveal any rearrangements in the genes for CSF-1 or the CSF-1R. Studies in humans have shown that patients with AML possess elevated levels of circulating CSF-1 and that AML cells can express CSF-1 and the CSF-1R. Thus, RI-AML in the SJL/J mouse appears to be a useful model for human AML.
Many events and requirements of the developmental program of human hematopoietic stem cells have not yet been discovered. A major impediment has been the lack of an appropriate experimental system. At present the conditions for maintaining human stem cells in vitro are not fully known. As a result within a short period the small stem cell pool is lost due to differentiation, making it difficult to examine the correlation between these cells and their function in vivo. Most of our knowledge of hematopoietic stem cells is from animal models in which purified stem cell canididates are assayed based on their functional ability to rescue lethally conditioned recipients. The permanent correction of many genetic disorders of the hematopoietic system requires efficient methods for introducing genes into stem cells in vitro. However, progress has been hindered by the absence of preclinical models that assay the repopulating capacity of primitive human cells. In addition, the development of therapy for malignant diseases also requires assays to identify the target leukemic stem cells based on their ability to initiate the disease. The recent development of methods to transplant or implant both normal and leukemic cells into immune-deficient mice provides the foundation for human stem cell assays. These models assay the repopulating capacity of primitive human cells and provide an important approach to identify and characterize human stem cells, both normal and leukemic. This review focuses on the development of functional assays for normal and leukemic human stem cells and on the new insights that these models are beginning to provide on the organization of the human stem cell hierarchy.
1996
The development of stem-cell gene therapy is hindered by the absence of repopulation assays for primitive human hematopoietic cells. Current methods of gene transfer rely on in vitro colony-forming cell (CFC) and long-term culture-initiating cell (LTC-IC) assays, as well as inference from other mammalian species. We have identified a novel human hematopoietic cell, the SCID-repopulating cell (SRC), a cell more primitive than most LTC-ICs and CFCs. The SRC, exclusively present in the CD4+CD8- fraction, is capable of multilineage repopulation of the bone marrow of nonobese diabetic mice with severe combined immunodeficiency disease (NOD/SCID mice). SRCs were rarely transduced with retroviruses, distinguishing them from most CFCs and LTC-ICs. This observation is consistent with the low level of gene marking seen in human gene therapy trials. An SRC assay may aid in the characterization of hematopoiesis, as well as the improvement of transduction methods.Errata: The abstract incorrectly stated that the SCI D-repopulating cells were exclusively present in the CD4'CD8 fraction; they were exclusively in the CD34'CD38 fraction. We regret the error.
Progress in understanding the abnormal regulation of hematopoiesis in chronic myelogenous leukemia (CML) would be facilitated if neoplastic sells, at all stages of the disease, could be studied in an animal model. In this report, we show that irradiated severs combined immunodeficient (SCID) mice can be transplanted with both normal (Philadelphia chromosome [Ph]-negative) and neoplastic (Ph+) cells from CML patients with either chronic or blast phase disease. Mice transplanted with peripheral blood (PB) or bone marrow (BM) cells from 9 of 12 chronic phase CML patients were well engrafted with human cells including multilineage colony-forming progenitors and CD34+ cells for at least 90 days posttransplantation. Repeated posttransplant injections of cytokines did not enhance the number of engrafted human cells. Interestingly, approximately 70% of the human progenitors found in the engrafted SCID BM were Ph-, suggesting that the growth of primitive normal cells is favored in this in vivo transplant model. A similar number of normal cells were found in mice transplanted with either PB or BM cells, suggesting that elevated numbers of primitive normal cells are present in CML PB. When cells from patients with CML in either myeloid or lymphoid blast crisis were transplanted into SCID mice, the BM of these mice was more rapidly repopulated and to a higher level than that observed with transplants of chronic phase cells. Moreover, all human colony-forming progenitors present in the BM of mice transplanted with blast crisis calls were Ph+, and the majority of cells showed the same morphological features of the blast crisis cells originally transplanted. These experiments provide a starting point for the creation of an animal model of CML and establish the feasibility of using this model for the future characterization of transplantable CML stem cells during disease progression.
1994
Unseparated or Ficoll-Hypaque (Pharmacia, Piscataway, NJ)-fractionated human cord blood cells were transplanted into sublethally irradiated severe combined immunodeficient (SCID) mice. High levels of multilineage engraftment, including myeloid and lymphoid lineages, were obtained with 80% of the donor samples as assessed by DNA analysis, fluorescence-activated cell sorting (FACS), and morphology. In contrast to previous and concurrent studies with adult human bone marrow (BM), treatment with human cytokines was not required to establish high-level human cell engraftment, suggesting that neonatal cells either respond differently to the murine microenvironment or they provide their own cytokines in a paracrine fashion. Committed and multipotential myelo-erythroid progenitors were detected using in vitro colony assays and FACS analysis of the murine BM showed the presence of immature CD34+ cells. In addition, human hematopoiesis was maintained for at least 14 weeks providing further evidence that immature hematopoietic precursors had engrafted the murine BM. This in vivo model for human cord blood-derived hematopoiesis will be useful to gain new insights into the biology of neonatal hematopoietic cells and to evaluate their role in gene therapy. There is growing evidence that there are ontogeny-related changes in immature human hematopoietic cells, and therefore, the animal models we have developed for adult and neonatal human hematopoiesis provide useful tools to evaluate these changes in vivo.
MOST human acute myeloid leukaemia (AML) cells have limited proliferative capacity, suggesting that the leukaemic clone may be maintained by a rare population of stem cells1-5. This putative leukaemic stem cell has not been characterized because the available in vitro assays can only detect progenitors with limited proliferative and replating potential4-7. We have now identified an AML-initiating cell by transplantation into severe combined immune-deficient (SCID) mice. These cells homed to the bone marrow and proliferated extensively in response to in vivo cytokine treatment, resulting in a pattern of dissemination and leukaemic cell morphology similar to that seen in the original patients. Limiting dilution analysis showed that the frequency of these leukaemia-initiating cells in the peripheral blood of AML patients was one engraftment unit in 250,000 cells. We fractionated AML cells on the basis of cell-surface-marker expression and found that the leukaemia-initiating cells that could engraft SCID mice to produce large numbers of colony-forming progenitors were CD34+CD38-; however, the CD34 +CD38+ and CD34- fractions contained no cells with these properties. This in vivo model replicates many aspects of human AML and defines a new leukaemia-initiating cell which is less mature than colony-forming cells.
1993
The possible participation of T cells in the promotion of hematopoietic engraftment of BM allografts, as opposed to their potential role in overcoming host-versus-graft reactions, was investigated recently by using (host X donor)F1 T cells devoid of graft-versus-host activity. In the present study, we provide further evidence of this effect by using tolerized thymocytes from established allogeneic chimeras. We show that tolerant mature thymocytes from donor type (C57BL/6 → C3H/HeJ) or host type (C3H/HeJ → C57BL/6) chimeras are as effective as (donor X host)F1 thymocytes in promoting both short-term and long-term engraftment of C57BL/6-Nu/Nu T cell-depleted BM cells in lethally irradiated C3H/ HeJ recipients.
1992
Transplantation of T-cell-depleted C57BL/6-Nu/Nu ("nude") bone marrow (BM) into C3H/HeJ recipients, conditioned with 8 Gy total body irradiation plus chemotherapy with the myeloablative drug dimethyl myleran, resulted in poor hematopoietic reconstitution 14 days posttransplant, compared with transplantation with T-cell-depleted BM from normal C57BL/6 donors. Hematopoietic reconstitution of "nude" BM could be improved by the addition of (C57BL/6xC3H/HeJ)F1 thymocytes void of graft-versus-host activity. Enhancement of BM allografting by thymocytes is sensitive to low radiation doses (≥5.0 Gy) and can be achieved by transplanting the BM 24 hours before the administration of thymocytes. Fractionation of F1 thymocytes by differential agglutination with peanut agglutinin (PNA) and by fluorescence activated cell sorting showed that this hematopoietic enhancing activity is enriched in the unagglutinated (PNA-) thymocyte fraction and is mediated by PNA- CD8+ and not by PNA- CD4+ thymocytes.
1991
Bone marrow samples from patients with pre-B acute lymphoblastic leukemia (pre-B ALL), either at diagnosis or at relapse, were transplanted into scid mice to determine whether these freshly obtained leukemic cells could proliferate in vivo and whether there were any differences in their in vivo growth characteristics. Cells from three patients who relapsed within 13 months of diagnosis proliferated rapidly in the murine bone marrow, spleen, and thymus, invaded peripheral organs, and resulted in morbidity and mortality of the animals within 4 to 16 weeks. Cells from two patients who relapsed 3.5 years after diagnosis grew much slower than the early relapse samples, taking up to 30 weeks to infiltrate the bone marrow of recipient mice. In contrast, leukemic cells were absent or were detected at low numbers in scid mice transplanted with cells obtained at diagnosis from three patients who have not yet relapsed. These results show an increased ability of leukemic cells from patients with aggressive lymphoblastic leukemia of poor prognosis to proliferate in scid mice.
The successful engraftment of human hematopoietic cells into immune-deficient mice offers a novel approach to characterize the developmental program of human hematopoiesis. While it is not yet possible to achieve high level engraftment of all human lineages, several methods have been developed to successfully engraft human lymphoid cells and reconstitute partial immune function. In addition to mature cell types, there is evidence that progenitors and perhaps stem cells can engraft the murine bone marrow. Recent work suggests that provision of exogenous human cytokines significantly increases the level of human cell engraftment and stimulates the development of multiple lineages. Progress has been made to establish animal models of human hematopoietic disease such as leukemia, autoimmunity, and infectious diseases. One major challenge for the future will be reconstitution of mice with the entire human hematopoietic system.
1988
C3H/HeJ mice were exposed to 8 or 9 Gy total body irradiation prior to transplantation of 1-15 x 106 H-2 incompatible T cell-depleted bone marrow cells from C57BL/6 donors. Survival was greatly enhanced compared to irradiated controls, even at the lowest cell doses. Analysis of spleen cells 1-7 weeks post-transplant revealed that recipients of the lowest doses of T cell-depleted bone marrow had only transient engraftment of donor type cells, and that long-term recovery was autologous. This transient engraftment had a marked beneficial effect both on reconstitution of hematopoiesis and on survival.
1987
Host-vs-graft activity presents a major obstacle for transplantation of T cell-depleted bone marrow in HLA-mismatched patients. In a primate model, conditioned exactly like leukemia patients, it was shown that residual host clonable T cells, as well as alloreactive cytotoxic precursors, were present in peripheral blood and spleen after completion of cytoreduction. We have now extended this study in a mouse model for allogeneic bone marrow transplantation. C3H/HeJ mice were treated by 9 Gy total body irradiation (TBI), and 24 hr later their spleen cells were cultured in the presence of T cell growth factor and phytohemagglutinin according to the limit dilution procedure. After 7 days of culture the average frequency of clonable cells was 2.5 X 10(-3) compared with 37 X 10(-3) in the spleens of normal mice. The T cell derivation of the growing cells was ascertained by complement-mediated cytotoxicity with anti-Thy-1 as well as with anti-Lyt-2 and anti-Ly-3T4. In parallel, we found that the initial engraftment rate of bone marrow allograft in mice given 9 Gy TBI was lower than that found in recipients of syngeneic marrow. The initial engraftment rate was measured by the number of colony-forming units in the spleen and by splenic uptake of 125IUdR. A slight increase in TBI from 9 Gy to 11 Gy markedly reduced the difference in the number of spleen colony-forming units or the IUdR uptake between recipients of allogeneic and syngeneic bone marrow. This increase in TBI also coincided with eradication of detectable clonable T cells. Moreover, in mice transplanted with T cell-depleted bone marrow after 9 Gy TBI, we also demonstrate that cytotoxicity against donor-type target cells is present in the spleen 10 to 14 days posttransplantation, whereas in mice treated by 11 Gy TBI such alloreactivity could not be detected. These results suggest that resistance to T cell-depleted allogeneic bone marrow in irradiated mice closely correlates with the frequencies of residual host clonable T cells detectable by conventional immunologic assays.