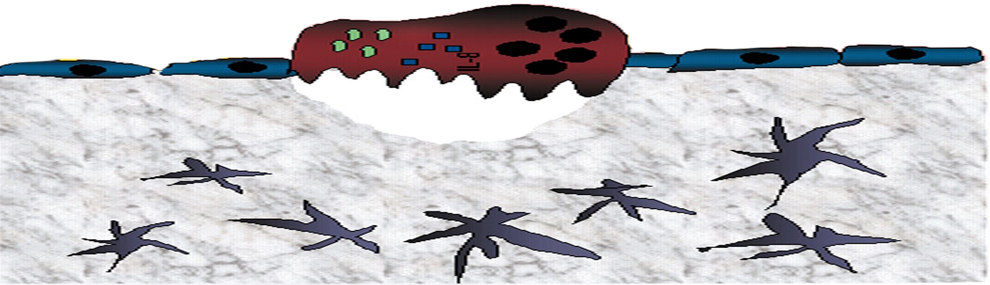
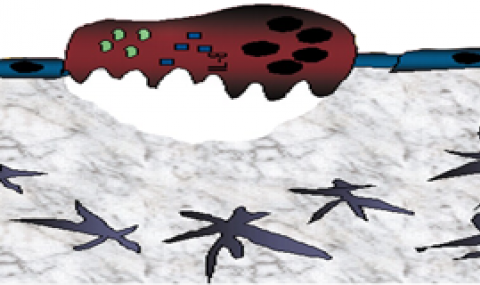
The majority of adult, long-term repopulating hematopoietic stem cells (LT-HSCs) are retained in the bone marrow (BM) in a quiescent non-motile mode via adhesive interactions which protect them from chemotherapy-induced DNA damage and lethal hematological failure. However, BM retained HSCs must proliferate and differentiate for homeostatic and stress-induced blood cell production on demand through life. Recently we discovered that factors, traditionally viewed as coagulation- and inflammation-related, also independently regulate mouse bone-marrow LT-HSC retention and recruitment to the blood via distinct protease activated receptor 1 (PAR1) signaling pathways. BM retained LT-HSC functionally express endothelial protein C receptor (EPCR) and PAR1 which induce their adhesion, while thrombin/PAR1 signaling induces EPCR shedding and HSC recruitment to the blood (Gur-Cohen S. et al Nature Medicine 2015). Herein we aim to decipher whether PAR1 surface expression levels can serve as a predictive factor for mobilization efficiency of human CD34+ HSC among healthy BM donors in clinical G-CSF-induced HSC mobilization for matched allogeneic transplantations.
Fourteen healthy donors were enrolled in our research. We found that PAR1 expression on circulating leukocytes before G-CSF treatment positively correlated with higher yields of mobilized leukocytes after stimulation (P=0.024). In addition, the percentage of PAR1-expressing CD34+ HSC in the blood and their absolute numbers before treatment also positively correlated with peripheral blood leukocyte count (P=0.003) and yield of mobilized CD34+ HSC.
Importantly, tracing the consequences of the follow up bone marrow transplantation, we raveled accelerated neutrophil engraftment and higher platelet counts (p=0.001) in patients transplanted with mobilized cells expressing higher surface PAR1 levels at baseline and after G-CSF stimulations. To better evaluate the role played by the PAR1 axis in regulation of G-CSF-induced HSC mobilization, we blocked PAR1 signaling in mice treated with G-CSF for 5 days. Co-administration of G-CSF with PAR1 antagonist abrogated HSC mobilization, concomitantly with increased numbers of bone forming mesenchymal progenitors as well as accumulation and expansion of BM EPCR+ LT-HSC.
Taken together, we report a crucial role for PAR1 signaling in mediating stem and progenitor cell (HSPC) mobilization during clinical G-CSF mobilization. Importantly, PAR1 expression by donor peripheral blood CD34+ HSPC before and after G-CSF administration can predict CD34+ HSC yields and moreover, neutrophil and platelet repopulation kinetics. Our study identifies PAR1 as an essential regulator of human G-CSF induced HSPC mobilization and provides new tools and knowledge that might lead to improved clinical stem cell mobilization and transplantation protocols.