Neutrophils are best known as glycolytic cells and an essential first host defense line of the innate immune system during inflammation. Activation of pro-inflammatory signaling by immune cells accelerates metabolic pathways, leading to increased lactate production. While lactate levels are the best clinical marker for sepsis diagnosis, the mechanisms underlying lactateproduction by bone marrow (BM) neutrophils and its role during inflammation remain poorly understood. Here, we report that LPS exposure in mice (mimicking bacterial inflammation) activated BM neutrophils leading to their mobilization to peripheral blood (PB) and recruitment to the liver. This happened concomitantly with an increase in BM neutrophil metabolism, reflected by high glucose uptake, high generation of reactive oxygen species (ROS) and increase in HIF-1α expression. Importantly, we identified that BM neutrophils highly express lactate dehydrogenase A (LDHA), an enzyme that converts pyruvate to lactate, as well as the lactate efflux transporter MCT4. On the other hand BM neutrophils express low levels of the lactate influx transporter MCT1 and the lactate receptor GPR81. In addition, we found that BM neutrophil depletion resulted in lower levels of BM derived lactate in mice exposed to LPS. Moreover, LPS administration up-regulated the expression of LDHA and MCT4 on BM neutrophils. Taken together, these results reveal that during acute LPS induced inflammation BM neutrophils produce and release high levels of lactate. Unexpectedly, we found that in vivo lactate treatment specifically induced rapid ROShigh neutrophil activation and mobilization from the BM to PB and liver in an NADPH oxidase/ROS dependent manner.
Accordingly, reduced activated neutrophil levels in PB and liver were observed following inhibition of ROS production. Furthermore, in a genetic mouse model of Chronic Granulomatous Disease (CGD) due to NADPH oxidase inactivation, with reduced ROS generation, treatment with lactate partially reduced neutrophil mobilization from the BM. Our results demonstrate that NADPH oxidase/ROS signaling play a role in lactate-induced neutrophil mobilization. HIF-1α is a major regulator of energy metabolism and glycolysis pathway in immune cells (Reviewed by Weidemann and Johnson, Cell Death and Diff. 2008, and by O’Neill and Pearce, J. Exp. Med. 2015). Notably, our results show in myeloid specific HIF-1α-deficient mice exposed to LPS a reduction in the expression of LDHA and MCT4 on BM neutrophils compared to wild type mice, suggesting that HIF-1α is upstream of lactate. Accordingly, exogenous lactate administration restored neutrophil mobilization in myeloid HIF-1α-deficient mice implicating HIF-1α in lactate production and release by BM neutrophils and in their mobilization from the BM following acute inflammation.
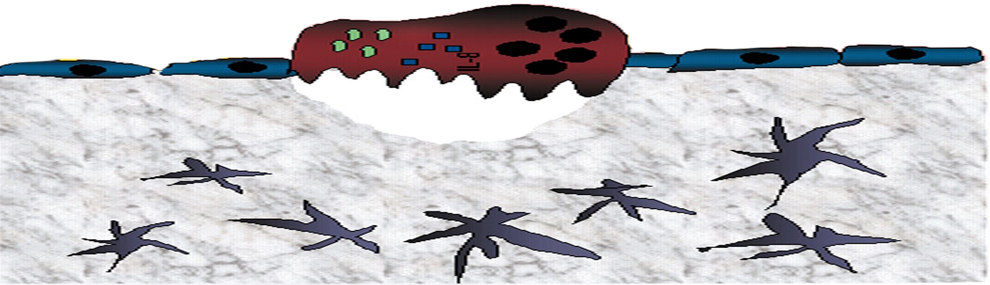
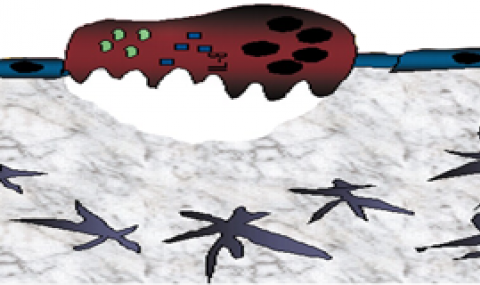
Further deciphering the mechanisms of lactate-induced neutrophil mobilization, we identified that BM endothelial cells (BMEC) highly express the lactate receptor GPR81. This GPCR was downregulated and internalized by lactate, as well as GPR81 agonist or LPS treatment. Interestingly, we found that lactate or GPR81 agonist reduced BMEC VE-Cadherin expression, leading to increased blood-BM vascular permeability as a possible cause for the enhanced neutrophil mobilization from the BM into the circulation. Lactate effects on BM neutrophils required functional GPR81 signaling since lactate injection together with a GPR81 antagonist, or to GPR81-deficient mice interfered with BM vascular permeability and reduced neutrophil mobilization from the BM. Moreover, in chimeras of GPR81-deficient BM reconstituted in wild type mice recipients we found that lactate induced-neutrophil mobilization is dependent on host BMEC GPR81 signaling rather than hematopoietic cell GPR81. This finding eludes to a role of endothelial GPR81 rather than to neutrophil GPR81 in lactate induced-neutrophil mobilization. In summary, our study links, for the first time, the metabolic by-product lactate secreted by BM neutrophils exposed to inflammatory conditions, to a novel GPR81 signaling axis on the BM endothelial cells which controls vascular permeability and thereby neutrophil mobilization. Our study highlights lactate as a potential target for attenuating blood neutrophilia and neutrophil injury associated with sepsis and other infectious conditions.