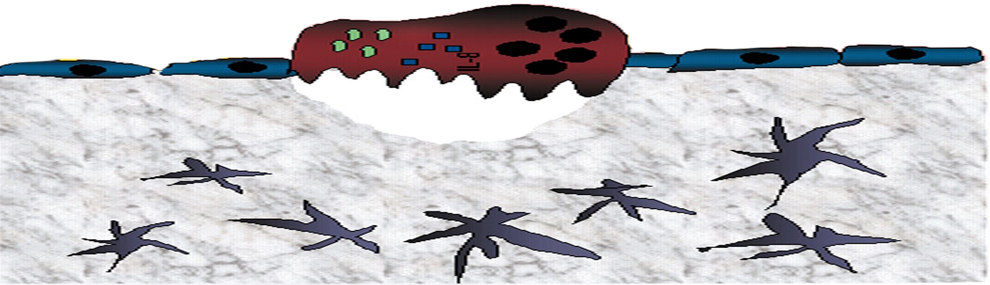
Hematopoietic stem and progenitor cell (HSPC) egress from the bone marrow (BM) to the circulation is tightly regulated and is accelerated during stress conditions, a process utilized for BM harvest. Recently, we demonstrated that mouse long term repopulating hematopoietic stem cell (LT-HSC) BM retention and their rapid release to the blood circulation are governed by a switch in nitric oxide (NO) generation via distinct coagulation-related protease activated receptor 1 (PAR1) cascades (Gur-Cohen S. et al., NM, 2016).
Herein we report that surface PAR1 expression can be exploited and serve as a positive predictive marker for the efficiency of human CD34+ HSPC mobilization among healthy donors in clinical G-CSF-induced mobilization for matched allogeneic transplantations. We found that PAR1 expression on circulating leukocytes before G-CSF administration was positively correlated with higher yields of mobilized leukocytes after stimulation (P0.5 x 109 /L) from an average of 14.6 days to an average of 11 days post-transplant. In addition, a trend of accelerated platelet production was documented to be related with higher PAR1 expression by circulating leukocytes prior to G-CSF stimulation. Consequently, poor mobilizer donors were characterized by extremely low surface PAR1 expression on circulating CD34+ cells prior to G-CSF stimulations. Herein we present a case report of a thrombophilic donor carrying the MTHFR mutation, expressing exceedingly low PAR1 levels at baseline, with the outcome of inadequate numbers of mobilized CD34+ HSPC in the blood following G-CSF treatments.
To further gain insight into the role played by PAR1 signaling in the regulation of G-CSF-induced HSPC mobilization, we used mice as a functional preclinical small animal model. We found that antagonizing PAR1 signaling attenuated both steady state release and G-CSF-induced HSPC mobilization. Furthermore, co-administration of G-CSF with PAR1 antagonist attenuated secretion of BM stromal CXCL12 and abrogated upregulation of surface CXCR4 and PAR1 expression by BM HSPCs, all leading to significantly reduced HSPC migration, differentiation and mobilization. In support, PAR1-/- mice failed to efficiently mobilize HSPCs in response to G-CSF compared to wild type counterparts. Enforced HSPC recruitment by G-CSF treatments dramatically accelerated PAR1-dependent NO production by eNOS, known to promote TACE-mediated EPCR shedding and rapid LT-HSC mobilization. Concomitantly, circulating steady state and G-CSF-mobilized stem cells lack surface EPCR expression. Intriguingly, while EPCR expression by primitive BM stem cells was transiently reduced after G-CSF treatments, antagonizing PAR1 signaling along with G-CSF stimuli blocked NO generation and synchronically expanded BM EPCR+ LT-HSC and their supportive stromal progenitor cells (MSPCs), as confirmed by increased repopulation in transplanted mice. Finally, we report an inverse PAR1 expression and regulation by BM HSPC and stromal MSPCs in mediating G-CSF-induced mobilization. G-CSF induced elevation of PAR1 expression on BM HSPCs, providing the driving force for their enhanced NO mediated migration, proliferation, differentiation and recruitment to the circulation. Contrary, the levels of PAR1 expression were reduced on MSPCs in response to G-CSF treatment, and following NO generation by eNOS activity and CXCL12 secretion, resulted in reduced mesenchymal differentiation leading to accumulated numbers of immature mesenchymal (CFU-F) and osteoblast (CFU-OB) progenitor cells .
Taken together, our study identifies and highlights inverse PAR1 signaling and NO generation as essential regulator of G-CSF induced HSPC mobilization and MSPC development opening new avenues to advance therapeutics for enhancing clinical G-CSF induced stem cell mobilization and transplantation protocols.