Pioneering work by Halberg in the 1960s showed increased susceptibility in mice injected with E. Coli endotoxin in the afternoon in contrast to mice injected with endotoxin from midnight. Recent findings have identified molecular mechanisms involved in the circadian regulation of a variety of immune progenitors, such as hematopoietic stem cells, and mature leukocytes, such as macrophages, as well as inflammatory cytokines. These oscillatory rhythms of immune cells and pro-inflammatory mediators, allow the host to anticipate and handle microbial threats more efficiently.
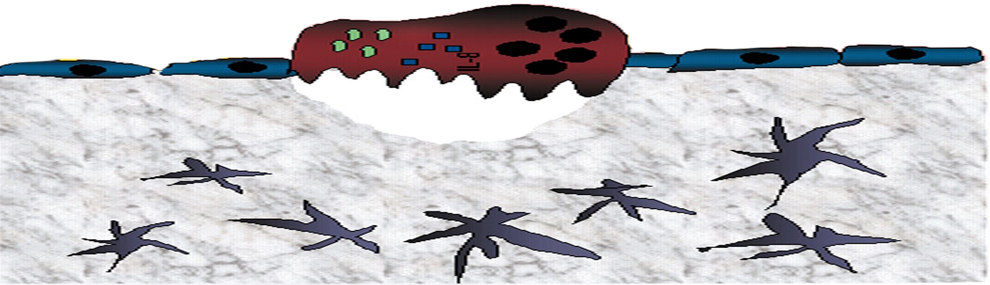
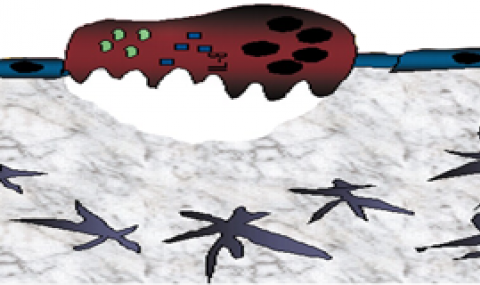
Golan et.al. (Cell Stem Cell, 2018) showed that murine bone marrow hematopoietic stem cells (HSC) primarily differentiate to mature leukocytes (neutrophils and monocytes) during the day. We suspect that this causes a hyper-inflammatory response in the day, therefore making mice more susceptible to bacterial endotoxins in the day (resting phase) compared to night (active phase). We investigate how the extent of the endotoxin response is regulated by diurnal oscillations in neutrophil phenotype and kinetics. Neutrophils act to resolve infection by phagocytosis, degranulation or the formation of neutrophil extracellular traps (NETs). Our preliminary results reveal that exposure to LPS at different times of the day affects neutrophil differently, leading dramatically elevated ROS production by neutrophils and increased mobilization of neutrophils and monocytes into circulation in the afternoon. This corresponds to a marked increase in the levels of pro-inflammatory cytokines in the blood in the afternoon, which may be lethal. But this is in sharp contrast to mice injected at midnight, where the number of activated neutrophils in PB reduce after LPS treatment- due to a significant reduction in BM vascular permeability, probably due to the high levels of the darkness hormone melatonin at night. Building on these findings, we expect that mice with a high neutrophil oxidative burst develop an exaggerated inflammatory response to LPS, and subsequently, higher mortality. We aim to provide mechanistic insights into the role of neutrophils and their effector molecules in regulating this process.