MicroRNAs (miRNAs) are small non-coding RNAs involved in various physiological processes, including hematopoiesis. Although miRNAs are broadly studied with regards to normal and malignant leukocyte development, the role of miRNAs in hematopoietic stem and progenitor (HSPC) migration and mobilization is poorly understood. Currently, induction of HSPC mobilization from the bone marrow (BM) to the peripheral blood (PB) is the major mean to harvest HSPCs for clinical transplantation. Recently, several miRNAs were found to be upregulated in macaque G-CSF-mobilized CD34+ HSPCs, among them the oncogenic miRNA mir-155 (Donahue et al., Blood 2009).
To study the involvement of mir-155 in HSPC regulation, we examined hematopoiesis in mir-155 knock out (KO) mice. Of interest, mir-155 KO mice had normal BM and PB levels of mature cells, but reduced levels of immature BM Lineage-/Sca-1+/c-Kit+ (LSK) and primitive BM CD34-LSK HSPCs. Profiling of mir-155 expression in murine hematopoietic BM populations, following G-CSF treatment, revealed differential expression patterns in wild type (WT) mice. G-CSF treatment upregulated mir-155 levels in immature LSK cells, in T-cells and in Mac-1+/Gr-1+ monocyte/macrophages. In contrast, G-CSF downregulated mir-155 levels in common lymphoid progenitors and in B-cells. Suggesting that mature hematopoietic cells may also participate in HSPC mobilization process. G-CSF administration to mir-155 KO mice resulted in reduced HSPC mobilization, as assessed by CFU-C and LSK cell counts in the PB. Surprisingly, G-CSF treatment increased BM LSK cell frequency in mir-155 KO mice to the same levels as in WT mice. On the contrary, G-CSF treatment reduced BM CD34-LSK cell frequency in WT mice and increased it in mir-155 KO mice showing an opposing effect on the more primitive HSPC population. Since mir-155 is involved also in mesenchymal development regulating osteoblast differentiation, we propose that BM HSPC pool reduction could be mediated by the stromal microenvironment. Additionally, osteoblasts and other BM residing cells undergo substantial changes in response to G-CSF that might be mediated by mir-155.
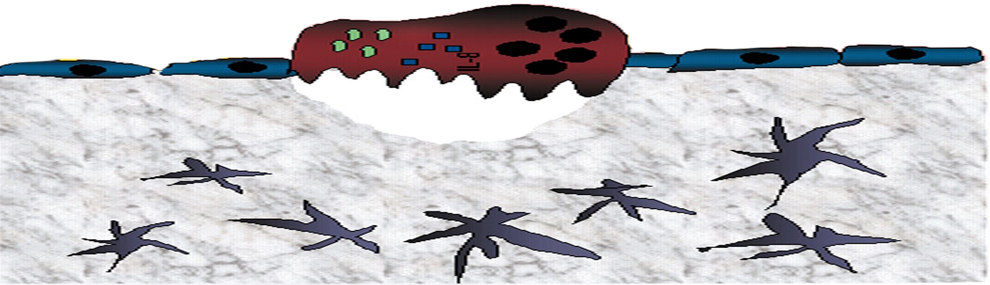
To determine whether the mobilization defect is hematopoietic cell-autonomous or due to an abnormal microenvironment, we examined G-CSF-induced mobilization in chimeric mice. Mir-155 KO mice reconstituted with wild type (WT) BM cells had normal mobilization as WT mice reconstituted with WT BM cells. Of interest, WT mice reconstituted with mir-155 KO BM cells showed reduced mobilization as mir-155 KO mice reconstituted with mir-155 KO BM cells. These results indicate that the mobilization defect in mir-155 KO mice is also due to a defect in HSPC motility. Since the CXCL12/CXCR4 axis plays a major role in HSPC mobilization, we examined the ability of mir-155 KO cells to perform CXCL12-induced migration and found reduced migration capacity of HSPCs in vitro. Although having reduced migration potential, mir-155 KO LSK cells had normal CXCR4 expression levels, suggesting that an aberrant intracellular response to SDF-1 is responsible for the observed defect. In support, AMD3100 treatment to mir-155 KO mice resulted in reduced HSPC rapid mobilization. Since SHIP-1 phosphatase mRNA is targeted by mir-155 in hematopoietic cells (Costinean et al., Blood 2009) and SHIP-1 KO hematopoietic cells exhibit increased migration towards CXCL12 (Kim et al., JCI 1999), we examined intracellular SHIP-1 expression during HSPC mobilization. SHIP-1 levels were downregulated in WT BM LSK cells in response to G-CSF or AMD3100 mobilizing treatments. In contrast, mir-155 KO BM LSK cells upregulated SHIP-1 levels in response to the mobilizing treatments. These results suggest that mir-155 may promote HSPC mobilization and increased motility via SHIP-1 downregulation.
In summary, our data indicates that mir-155 directly promotes HSPC motility and mobilization by SHIP-1-mediated regulation of intracellular response to CXCL12 signaling. We also propose the mechanism of indirect regulation of BM HSPC pool size during steady state and following G-CSF treatment by mir-155, via stromal BM microenvironment, which is currently under investigation. Deciphering the mechanisms of HSPC migration and maintenance in general and by mir-155 in particular, may potentially improve clinical mobilization protocols and contribute to increased donor BM engraftment following transplantation.