Bone marrow (BM) endothelial cells (BMECs) form a network of blood vessels (BVs) that regulate both leukocyte trafficking and hematopoietic stem and progenitor cell (HSPC) maintenance.
However, it is not clear how BMECs balance between these dual regulatory roles and if these events occur at the same vascular site. We define the BM architecture of functionally distinct BVs, their spatial localization and association with specific stromal precursors, which cooperatively regulate HSPC fate. BM stem and progenitor cell maintenance in a metabolically nonactive state and leukocyte trafficking occur at separate sites and are differentially regulated by specific BVs with distinct permeability properties.
BM arteries were found to be mostly encircled by aSMA + pericytes whereas the ensuing smalldiameter endosteal and trabecular arterioles were predominantly surrounded by stem cellniche supporting stromal precursor cells. Live imaging and flow analysis revealed that endosteal arteriole BVs exhibited high flow rate, low permeability to external plasma from the peripheral blood, and high levels of adhesion and tightjunction molecules.
Primitive HSPCs located in periarteriole regions were found in a nonactivated, low reactive oxygen species (ROS) state. Exposure of BM HSPCs to peripheral blood plasma, enhanced their metabolic activity, exhibited by enhanced intracellular ROS levels, and glucose uptake.
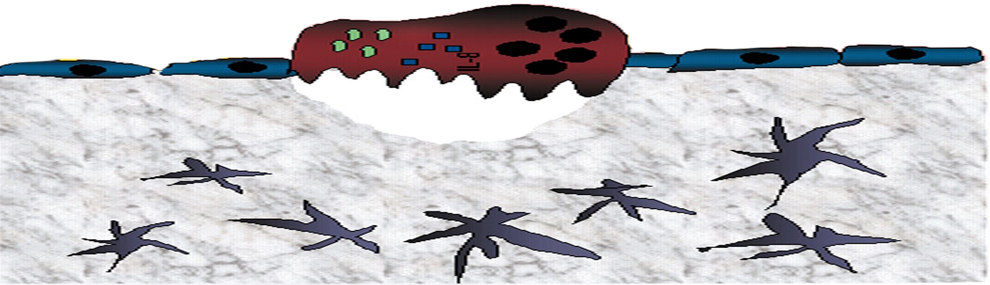
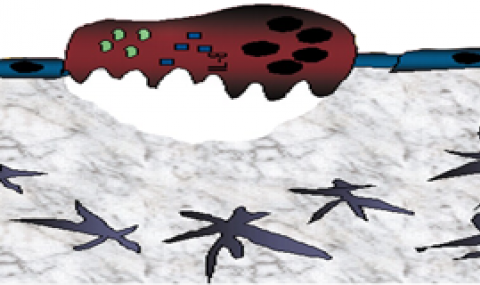
The same was also evident for circulating HSPCs in the blood. Plasmaexposed HSPCs displayed enhanced motility alongside with reduced longterm repopulation potential. Live imaging showed that all immature and mature leukocyte bidirectional trafficking occurred exclusively at the more permeable sinusoids, located downstream to the endosteal arterioles. Of note, BM sinusoids contained a higher prevalence of ROS high cells in their microenvironment, including HSPCs.
Rapid AMD3100 induced HSPC mobilization preferentially affected sinusoidal but not arterial BVs permeability and CXCL12 chemokine release. Endothelial specific in vivo interference with CXCL12CXCR4 interactions, via conditional CXCR4 genetic deletion, hampered BM barrier integrity resulting in enhanced HSPC egress. In line with these results we found that during conditions favoring BM stem and progenitor cells expansion, endothelial integrity was enhanced along with reduced HSPC bidirectional trafficking.
Conversely, conditional endothelial specific induced genetic or pharmacologic disruption of barrier integrity augmented ROS levels in HSPCs, enhancing their bidirectional trafficking and differentiation while reducing their BM pool size and maintenance in a metabolically nonactive state. Of note, humanized mice engrafted with preB ALL cells exhibited reduced BM barrier permeability most probably due to BM endothelium modification via FGF2 secretion by the leukemic clone.
Interestingly, human preB ALL cells displayed hypersensitivity to plasmatic exposure. We hypothesize that malignant cells modify BM endothelium to provide themselves with a supportive and protective microenvironment composed of undifferentiated BM stromal progenitors and tightly sealed endothelial barrier. In conclusion, our study identifies anatomically distinct BM BVs with different barrier functions serving as systemic leukocyte trafficking or HSPC BM maintenance sites with clinical therapeutic relevance.